肾小球足细胞数量减少与CKD进展有关
IF 5.7
2区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
摘要
足细胞耗竭可能在慢性肾脏疾病(CKD)中起重要作用;然而,缺乏对无肥胖相关性肾小球病变人群的纵向临床研究。方法研究的患者在2000年至2021年间接受了根治性肾切除术,组织学上有10%的间质纤维化和肾小管萎缩(IFTA)。通过透析、肾移植、持续估计肾小球滤过率(eGFR)≤10 ml/min / 1.73 m2或肾切除术后基线eGFR持续下降30%来确定进展性CKD的病例。在相同的随访时间,每个进行性CKD病例的年龄性别与没有进行性CKD的对照组相匹配。用免疫组织化学和体视学测定足量测量(数量/肾小球、密度和细胞体积)和壁上皮细胞(PEC)测量(数量/肾小球和密度)。通过足部测量评估进展性CKD的风险,调整肾小球丛体积、肾小球硬化、IFTA和动脉硬化(全部由形态学测定)或调整年龄、性别、糖尿病、体重指数(BMI)、高血压、eGFR和蛋白尿。结果CKD 35例,对照组35例。病例与对照组在BMI(平均:29.1 vs 28.2 kg/m2, P = 0.88)、肾小球簇体积或PEC数量方面无显著差异,但足细胞数量、足细胞密度和PEC密度较低。足细胞数量减少与几种肾硬化指标相关。在调整后的分析中,足细胞数量和足细胞密度与进行性CKD相关,并且这些关联在皮层深度上没有实质性差异。结论每肾小球足细胞数低与CKD进展相关,与CKD危险因素、肾功能、肾小球体积和肾硬化严重程度无关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Lower Podocyte Number per Glomerulus Associates With Progressive CKD
Introduction
Podocyte depletion may play an important role in chronic kidney disease (CKD); however, longitudinal clinical studies are lacking in populations without obesity-related glomerulopathy.
Methods
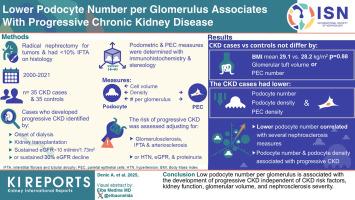
Patients studied underwent radical nephrectomy for tumors between 2000 and 2021 and had < 10% interstitial fibrosis and tubular atrophy (IFTA) on histology. Cases who developed progressive CKD were identified by the onset of dialysis, kidney transplantation, sustained estimated glomerular filtration rate (eGFR) < 10 ml/min per 1.73 m2, or sustained 30% eGFR decline after the postnephrectomy baseline eGFR. Each case of progressive CKD was age-sex-matched to a control without progressive CKD at the same follow-up time. Podometric measures (number/glomerulus, density, and cell volume) and parietal epithelial cell (PEC) measures (number/glomerulus and density) were determined with immunohistochemistry and stereology. The risk of progressive CKD with podometric measures was assessed, adjusting for glomerular tuft volume, glomerulosclerosis, IFTA, and arteriosclerosis (all determined by morphometry) or adjusting for age, sex, diabetes mellitus, body mass index (BMI), hypertension, eGFR, and proteinuria.
Results
There were 35 CKD cases and 35 controls studied. Cases versus controls did not differ significantly by BMI (mean: 29.1 vs. 28.2 kg/m2, P = 0.88), glomerular tuft volume, or PEC number, but had lower podocyte number, lower podocyte density, and lower PEC density. Lower podocyte number correlated with several nephrosclerosis measures. In adjusted analyses, podocyte number and podocyte density associated with progressive CKD and these associations did not substantively differ by cortex depth.
Conclusion
Low podocyte number per glomerulus is associated with the development of progressive CKD independent of CKD risk factors, kidney function, glomerular volume, and nephrosclerosis severity.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Kidney International Reports
Medicine-Nephrology
CiteScore
7.70
自引率
3.30%
发文量
1578
审稿时长
8 weeks
期刊介绍:
Kidney International Reports, an official journal of the International Society of Nephrology, is a peer-reviewed, open access journal devoted to the publication of leading research and developments related to kidney disease. With the primary aim of contributing to improved care of patients with kidney disease, the journal will publish original clinical and select translational articles and educational content related to the pathogenesis, evaluation and management of acute and chronic kidney disease, end stage renal disease (including transplantation), acid-base, fluid and electrolyte disturbances and hypertension. Of particular interest are submissions related to clinical trials, epidemiology, systematic reviews (including meta-analyses) and outcomes research. The journal will also provide a platform for wider dissemination of national and regional guidelines as well as consensus meeting reports.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


