美国东南部11个州规定燃烧产生的PM2.5与急诊室就诊之间的关系
IF 9.7
1区 环境科学与生态学
Q1 ENVIRONMENTAL SCIENCES
引用次数: 0
摘要
更长、更严重的野火季节正在成为火灾多发地区的常态。规定燃烧是一种用来减轻野火蔓延的工具。然而,规定燃烧也会造成空气污染,包括PM2.5(空气动力学直径 <;= 2.5 µm的颗粒物)。虽然野火烟雾(WFS)对健康的影响已经得到了充分的研究,但对规定火灾烟雾(PFS)的影响了解相对较少。我们的研究利用美国东南部11个州(2013-2021年)居民的医疗保健索赔来调查与PFS相关的健康影响。我们使用化学传输模型(CTM)和基于数据融合的方法来估计县级室外pfs特异性PM2.5浓度,并采用时间分层病例交叉设计来量化与PM2.5水平滞后0-3 天相关的急诊就诊相对风险。模型调整了非规定火灾PM2.5和O3,温度,湿度和假期。我们还研究了不同人群中相对风险的差异。pfs特异性PM2.5与非外因ED就诊的相对风险相关(1.01,95 %置信区间(CI): 1.01, 1.02),比较4.3 µg/m3(第95百分位数)和0 µg/m3,上呼吸道感染(1.04,95 % CI: 1.01, 1.07)和缺血性心脏病(1.06,95 % CI: 1.01, 1.11)。我们没有观察到总体呼吸结局、哮喘或COPD的风险增加,这与已发表的WFS研究结果不同。相对风险因结果而异,按年龄和社会脆弱性标记定义的人群亚组之间的相对风险略有不同。然而,经过多次比较校正后,这些差异并不显著。一些调查结果与以前在其他地方报道的关于WFS的关联不同,突出表明需要直接比较WFS与PFS对健康的影响,以评估作为火灾管理工具的规定燃烧的安全性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
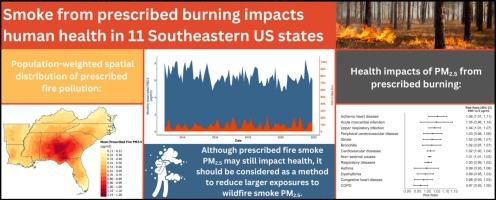
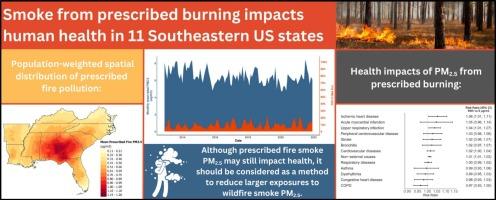
Associations between PM2.5 from prescribed burning and emergency department visits in 11 Southeastern US states
Longer, more severe wildfire seasons are becoming the norm in fire-prone areas. Prescribed burning is a tool used to mitigate wildfire spread. However, prescribed burning also contributes to air pollution, including PM2.5 (particulate matter with aerodynamic diameter <= 2.5 µm). While the health impacts of wildfire smoke (WFS) are well-studied, relatively less is known about the effects of prescribed fire smoke (PFS). Our study leverages healthcare claims available for residents of 11 Southeastern US states (2013–2021) to investigate the health impacts associated with PFS. We used a chemical transport model (CTM) and data fusion-based method to estimate county-level outdoor PFS-specific PM2.5 concentrations and employed a time-stratified case-crossover design to quantify the relative risk of emergency department (ED) visits associated with PM2.5 levels lagged 0–3 days. Models adjusted for non-prescribed fire PM2.5 and O3, temperature, humidity, and holidays. We also examined how relative risks varied across population subgroups. PFS-specific PM2.5 was associated with a relative risk of ED visits for non-external causes (1.01, 95 % confidence interval (CI): 1.01, 1.02) comparing 4.3 µg/m3 (95th percentile) versus 0 µg/m3, upper respiratory infections (1.04, 95 % CI: 1.01, 1.07), and ischemic heart disease (1.06, 95 % CI: 1.01, 1.11). We did not observe an increased risk for overall respiratory outcomes, asthma, or COPD, which differs from published WFS findings. Relative risks varied across outcomes and modestly across population subgroups defined by age and markers of social vulnerability. However, after correcting for multiple comparisons, these differences were not significant. Some findings differed from associations previously reported elsewhere for WFS, highlighting the need for direct comparisons of the health impacts of WFS versus PFS for evaluating safety of prescribed burning as a fire management tool.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Environment International
环境科学-环境科学
CiteScore
21.90
自引率
3.40%
发文量
734
审稿时长
2.8 months
期刊介绍:
Environmental Health publishes manuscripts focusing on critical aspects of environmental and occupational medicine, including studies in toxicology and epidemiology, to illuminate the human health implications of exposure to environmental hazards. The journal adopts an open-access model and practices open peer review.
It caters to scientists and practitioners across all environmental science domains, directly or indirectly impacting human health and well-being. With a commitment to enhancing the prevention of environmentally-related health risks, Environmental Health serves as a public health journal for the community and scientists engaged in matters of public health significance concerning the environment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


