早期血运重建对中度或重度缺血的稳定冠状动脉疾病的实际疗效
IF 1.8
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
American heart journal plus : cardiology research and practice
Pub Date : 2025-08-24
DOI:10.1016/j.ahjo.2025.100596
引用次数: 0
摘要
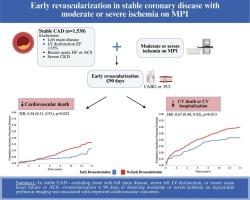
背景:比较有效性的研究可能为缺血试验对现实世界患者的推广提供见解。我们通过心肌灌注成像(MPI)评估了稳定型冠状动脉疾病患者在检测到中度或重度缺血后90天内进行血运重建术的长期疗效。方法选取2003年1月至2020年3月在某三级学术医疗中心连续接受单光子发射计算机断层扫描(MPI)的中重度缺血患者(总差值≥7分)。将MPI术后早期血运重建(定义为90天内经皮冠状动脉介入治疗或冠状动脉旁路移植术)与未进行早期血运重建的患者进行比较,但不包括左主干疾病、严重慢性肾脏疾病、严重左心功能障碍、近期急性冠状动脉综合征或心力衰竭住院的患者。主要结局是心血管死亡或心血管住院或心血管死亡的复合,并在整个省级医疗保健系统中进行跟踪。结果1530例患者(平均年龄65岁,男性70%)随访时间中位数为9.9年。经反概率加权治疗后,与不进行早期血运重建术治疗的患者相比,早期血运重建术患者心血管死亡风险较低(3.76% vs 8.93%; HR 0.54, 95% CI: 0.31-0.91, p = 0.022),复合终点降低(33.73% vs 43.94%; HR 0.67, 95% CI: 0.49-0.92, p = 0.013)。结论稳定期冠状动脉病变MPI术后出现中度或重度缺血的患者,与不进行早期血运重建术的患者相比,早期血运重建术的患者心血管死亡和心血管住院或心血管死亡的综合风险较低。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Real-world effectiveness of early revascularization in stable coronary artery disease with moderate or severe ischemia
Background
Comparative effectiveness studies may provide insights into generalizability of the ISCHEMIA trial to real-world patients. We evaluated the long-term effectiveness of revascularization within 90 days after detecting moderate or severe ischemia on myocardial perfusion imaging (MPI) in stable coronary artery disease.
Methods
All consecutive patients with moderate or severe ischemia (summed difference score ≥7) on single photon emission computed tomography MPI at a tertiary academic medical center were included (January 2003 to March 2020). Early revascularization (defined as percutaneous coronary intervention or coronary artery bypass grafting within 90 days) after MPI, was compared to those patients treated without early revascularization, excluding those with left main disease, severe chronic kidney disease, severe left ventricular dysfunction, recent acute coronary syndrome or heart failure hospitalization. Primary outcomes were cardiovascular death or the composite of cardiovascular hospitalization or cardiovascular death, and were tracked throughout the provincial healthcare system.
Results
1530 patients (mean age: 65 years; 70 % male) were followed for a median of 9.9 years. After inverse-probability treatment weighting, early revascularization was associated with lower risks of cardiovascular death (3.76 % vs 8.93 %; HR 0.54, 95 % CI: 0.31–0.91, p = 0.022) and a reduction in the composite endpoint (33.73 % vs 43.94 %; HR 0.67, 95 % CI: 0.49–0.92, p = 0.013) compared to those treated without early revascularization.
Conclusions
Patients with stable coronary artery disease treated with early revascularization after MPI showing moderate or severe ischemia experienced lower risks of cardiovascular death and composite of cardiovascular hospitalization or cardiovascular death compared to those treated without early revascularization.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American heart journal plus : cardiology research and practice
Cardiology and Cardiovascular Medicine
CiteScore
1.60
自引率
0.00%
发文量
0
审稿时长
59 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


