腹结核患者肝损伤模式及抗结核治疗的适应性:一项前瞻性队列研究
IF 3.2
Q2 GASTROENTEROLOGY & HEPATOLOGY
Journal of Clinical and Experimental Hepatology
Pub Date : 2025-08-05
DOI:10.1016/j.jceh.2025.103124
引用次数: 0
摘要
背景dextra -pulmonary tuberculosis与抗结核治疗(ATT)中药物性肝损伤(DILI)的高风险相关。然而,一些患者的肝功能障碍也可以由于肝适应(HA)而恢复正常。专门针对腹结核(ATB)患者这些问题的前瞻性数据缺乏。本研究旨在评估ATB患者接受at治疗后的肝损伤模式、HA及其预测因素。方法本研究是一项前瞻性队列研究,涉及140例ATB患者和正常基线肝功能检查(LFTs)。患者接受标准的四药联合化疗,并连续监测LFTs。采用多变量logistic回归评估预测因素。结果slft异常71例(50.7%)。其中20例(14.2%)在首次异常时符合DILI标准。其余51例进展为DILI 18例(35.3%),自发性消退33例(64.7%),与HA一致。总体而言,27.1%的患者发生DILI, 46.4%的LFT异常因HA而消退。大多数DILI(89%)发生在治疗的前8周,HA的中位时间为21天。低血清白蛋白和维生素D独立预测DILI进展。65.8%的病例成功完全重新引入ATT。吡嗪酰胺最常与重新引入失败相关。DILI病例均未发展为急性肝衰竭。结论接受ATT治疗的ATB患者中lft异常较为常见;然而,近一半的患者由于HA而自发消退。低白蛋白血症和维生素D缺乏独立预测DILI的进展,强调警惕LFT监测的必要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
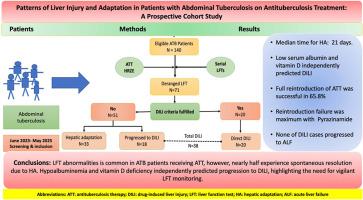
Patterns of Liver Injury and Adaptation in Patients With Abdominal Tuberculosis on Antituberculosis Treatment: A Prospective Cohort Study
Background
Extra-pulmonary tuberculosis is associated with a higher risk of drug-induced liver injury (DILI) with antituberculosis treatment (ATT). Nevertheless, hepatic dysfunctions in some patients can also regress to normalization due to hepatic adaptation (HA). Prospective data specifically addressing these issues in patients with abdominal tuberculosis (ATB) is lacking. This study was aimed to evaluate the patterns of hepatic injury, HA, and their predictors in patients with ATB receiving ATT.
Methods
This was a prospective cohort study involving 140 patients with ATB and normal baseline liver function tests (LFTs). Patients received standard four-drug ATT, and LFTs were serially monitored. Predictive factors were evaluated using multivariable logistic regression.
Results
LFT abnormalities occurred in 71 patients (50.7%). Of these, 20 (14.2%) met DILI criteria at first abnormality. Among the remaining 51, 18 (35.3%) progressed to DILI, while 33 (64.7%) showed spontaneous resolution, consistent with HA. Overall, 27.1% patients developed DILI, and 46.4% of LFT abnormalities resolved due to HA. The majority (89%) of DILI occurred within the first 8 weeks of treatment, and median time for HA was 21 days. Low serum albumin and vitamin D independently predicted DILI progression. Full reintroduction of ATT was successful in 65.8% of cases. Pyrazinamide was most commonly associated with reintroduction failure. None of DILI cases progressed to acute liver failure.
Conclusion
LFT abnormalities is common in ATB patients receiving ATT; however, nearly half experience spontaneous resolution due to HA. Hypoalbuminemia and vitamin D deficiency independently predicted progression to DILI, highlighting the need for vigilant LFT monitoring.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Clinical and Experimental Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.90
自引率
16.70%
发文量
537
审稿时长
64 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


