COPD患者静息能量消耗:预测方程与间接量热法之间的一致性
Q3 Nursing
引用次数: 0
摘要
准确、个性化的能量和蛋白质以及其他营养成分对于改善慢性阻塞性肺病患者的营养状况和增加肌肉质量非常重要,特别是那些营养耗尽和瘦体重减少的患者。尽管使用间接量热法(IC)具有很高的准确性,但能量需求的确定往往受到其可用性的限制,因此预测方程被用作替代方案。本研究旨在确定使用IC测量的REE与从临床实践中常用的COPD患者(无论有无营养不良或肌肉减少症)的预测方程中获得的估计REE之间的一致性。方法对2022年8月至2023年1月期间经临床和肺活量测定确诊的COPD患者进行横断面研究。对所有参与者进行IC、生物电阻抗分析、人体测量、握力测量以及生化测试(血清白蛋白、ESR和CRP),以收集数据分析两种方法之间的相关性和一致性。测试的预测方程包括哈里斯-本尼迪克特、斯科菲尔德、医学研究所、米夫林圣约尔、韦斯特普、森川和摩尔和安吉利洛方程。使用独立样本t检验和Mann-Whitney U检验对有和没有营养不良或肌肉减少症的组之间的能量消耗差异进行统计检验,同时使用Bland-Altman图分析和报告方法之间的相关性和一致性程度。显著双尾P值设为<;0.05。结果共纳入84例COPD患者(25%为女性)。平均年龄71±14岁。肺活量计平均值:FEV1/FVC为预测值61.5±9%,FEV1为预测值64±15%,FVC为预测值85.52±13.9%。COPD伴肌少症患者的平均REE明显低于无肌少症患者(1154±238 kcal/d vs 1230±234 kcal/d, P=0.01)。在有和没有营养不良或高炎症标志物的COPD患者之间,平均REE测量值无统计学差异。Bland-Altman图显示,在测试的方程中,使用Westerterp方程估计稀土元素的准确率最高(58.3%),其次是Scofield方程(57.1%),偏差和一致限分别为26 kcal/天,Westerterp方程为-288 ~ +340 kcal/天,Schofield方程为+32 kcal/天,-353 ~ +289 kcal/天。结论使用Schofield和Westerterp方程估算COPD患者的REE在不同的临床条件下具有较高的准确率和较低的偏倚水平,可用于无IC时的估算。当FFM测量可用时,Nordenson方程提供了最高的估计精度。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Resting energy expenditure in patients with COPD: Agreement between predicted equations and indirect calorimetry
Background
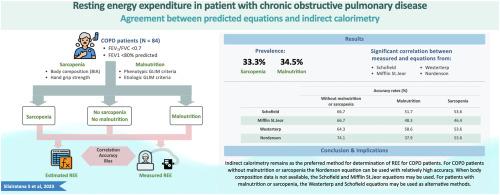
Accurate, individualized energy and protein, as well as other nutrient components, are highly important to improve the nutritional status and increase muscle mass in COPD patients, particularly those having nutritional depletion and experiencing a loss of lean body mass. Despite having a high degree of accuracy, the determination of energy requirement using indirect calorimetry (IC) is often limited by its availability and therefore predictive equations are used as alternatives. This study aims to determine agreements between measured REE using IC and estimated REE obtained from predictive equations that are commonly used in clinical practice among COPD patients, both with and without malnutrition or sarcopenia.
Methods
A cross-sectional study was conducted among clinically- and spirometry-confirmed COPD patients from August 2022 to January 2023. IC, bioelectrical impedance analysis, anthropometry, handgrip strength measurement as well as biochemical tests (serum albumin, ESR and CRP) were performed in all participants to collect data for analysis of correlation and agreement between two methods. The predictive equations tested included the Harris-Benedict, Schofield, Institute of Medicine, Mifflin St Jeor, Westerterp, Morikawa, and Moore & Angelilo equations. The differences of energy expenditure between groups with and without malnutrition or sarcopenia were tested statistically using an independent-sample t-test and Mann-Whitney U test, while correlations, as well as degree of agreement between methods were analyzed and reported using Bland-Altman plots. The significant two-tailed P value was set at <0.05.
Results
A total of 84 patients with COPD (25% women) were included in the study. the average age was 71±14 years. The average spirometric values were as follows: FEV1/FVC 61.5±9%, FEV1 64±15% of predicted, and FVC 85.52±13.9% of predicted. Among the COPD patients with sarcopenia, the average REE was significantly lower than patients without sarcopenia (1154±238 kcal/day vs 1230±234 kcal/day, P=0.01). No statistically significant differences of the average measured REE between COPD patients with and without malnutrition or high inflammatory markers was observed. Bland-Altman plots demonstrated that, among the equations tested, estimated REE using Westerterp equation provided the highest accuracy rate (58.3%) followed by the Scofield equation (57.1%) with the bias and limit of agreement of 26 kcal/day and -288 to +340 kcal/day for Westerterp and +32 kcal/day and -353 to +289 kcal/day for Schofield equation, respectively.
Conclusion
Estimation of REE using Schofield and Westerterp equation provides better accuracy rate and lower level of bias in COPD patients across various clinical conditions and may be used for estimation when IC is not available. When FFM measurement is available, Nordenson equation provide the highest accuracy of estimates.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Clinical Nutrition Open Science
Nursing-Nutrition and Dietetics
CiteScore
2.20
自引率
0.00%
发文量
55
审稿时长
18 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


