条件血浆促进大鼠模型全层皮肤缺损愈合
IF 3.5
3区 环境科学与生态学
Q3 CELL & TISSUE ENGINEERING
引用次数: 0
摘要
血液衍生物可以促进伤口愈合,但每一种都具有不同的特性,在患者治疗中产生不同的结果。本研究旨在研究使用聚乳酸(PLA)包被微球的条件血浆(CP)在急性伤口愈合中的疗效,并将其与使用裸微球和富血小板血浆(PRP)的条件血浆(CP)进行比较。方法采集7名自愿献血者的血液,分别装在ACD抗凝剂、PLA包被或裸珠的3支试管中,37℃孵育6 h。采用ELISA法检测VEGF、PDGF、TGF-β、IL-1β、IL-13、IL-1Ra的浓度。在大鼠背部做全层创面。PRP, CP与pla包覆珠或裸珠,磷酸盐缓冲盐水作为对照施用于创面。第3、7、10、14天伤口愈合率;术后14 d,观察大鼠上皮化、成纤维细胞、炎性细胞浸润、新胶原形成、新血管及免疫组化(CD31、α-SMA)的变化。结果CPs中VEGF、PDGF、TGF-β、il -1 -β、IL-1Ra浓度显著高于PRP (p < 0.05)。CP与pla包被珠促进伤口闭合,改善皮肤伤口愈合(p < 0.05),这与增强上皮化、成纤维细胞增殖、新胶原形成和减少炎症细胞浸润有关。免疫组化结果显示,各治疗组CD31和α-SMA水平较对照组升高,但差异无统计学意义(p > 0.05)。结论cp可促进创面上皮化、成纤维细胞增殖、胶原合成和沉积,减少炎症细胞浸润,促进创面愈合。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Conditioned plasma promotes full-thickness skin defect healing in a rat model
Introduction
Blood derivatives may enhance wound healing, but each possesses distinct characteristics and has yielded varying outcomes in patient treatment. This research seeks to examine the efficacy of conditioned plasma (CP) using polylactic acid (PLA) coated beads and to compare it with CP using bare beads and platelet-rich plasma (PRP) in the context of acute wound healing.
Methods
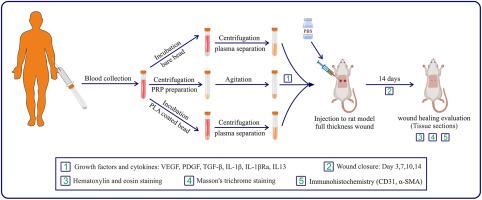
Blood was collected from 7 volunteer donors in three tubes containing ACD anticoagulant, PLA coated, or bare beads and incubated for 6 h at 37 °C. The concentration of VEGF, PDGF, TGF-β, IL-1β, IL-13, and IL-1Ra were measured by ELISA. Full-thickness wounds were made on the back of rats. PRP, CP with PLA-coated bead or bare beads, and phosphate buffer saline as control were administered to the wound area. Wound closure rate at days 3, 7, 10, and 14; epithelialization, fibroblast cells, inflammatory cells infiltration, new collagen formation, new vessel, and immunohistochemistry (CD31, α-SMA) were measured 14 days after the incision.
Results
The concentration of VEGF, PDGF, TGF-β, IL1-β, and IL-1Ra was significantly higher in CPs than in PRP (p < 0.05). CP with PLA-coated beads promoted wound closure and improved skin wound healing (p < 0.05), which was associated with enhanced epithelialization, fibroblast cell proliferation, new collagen formation, and reduced inflammatory cells infiltration. Immunohistochemistry showed an increase in CD31 and α-SMA levels in the treatment groups compared to the control group, but this increase was insignificant (p > 0.05).
Conclusion
CP promotes wound healing by increasing epithelialization, fibroblast proliferation, collagen synthesis and deposition, and reducing inflammatory cells infiltration.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Regenerative Therapy
Engineering-Biomedical Engineering
CiteScore
6.00
自引率
2.30%
发文量
106
审稿时长
49 days
期刊介绍:
Regenerative Therapy is the official peer-reviewed online journal of the Japanese Society for Regenerative Medicine.
Regenerative Therapy is a multidisciplinary journal that publishes original articles and reviews of basic research, clinical translation, industrial development, and regulatory issues focusing on stem cell biology, tissue engineering, and regenerative medicine.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


