92例T1壶腹癌切除术后的预后和复发模式。
IF 2.4
3区 医学
Q2 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
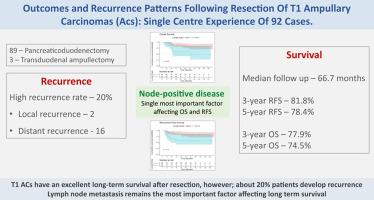
背景:切除的早期壶腹癌(T1)具有最佳的总生存期(OS),但与晚期壶腹癌和其他壶腹周围癌相比,其术后发病率更高。方法:回顾性分析2012年1月至2022年12月在孟买塔塔纪念中心切除的T1-ACs。评估围手术期和远期预后。结果:92例患者行T1-ACs切除术,显著发病率(Clavien-Dindo≥3)为38%,临床相关术后胰瘘发生率为22.5%。切除的T1-ACs的淋巴结阳性率为25%。3年和5年OS分别为77.9%和74.5%,无复发生存率(RFS)分别为81.8%和78.4%。在66.7个月的中位随访期间,有18例(19.6%)复发(2例局部,16例远处)。复发后3年和5年的OS分别为29.6%和14.8%。淋巴结转移是影响OS (HR 2.815, 95% CI: 1.114 ~ 7.112, p = 0.029)和RFS (HR 2.54, 95% CI: 0.978 ~ 6.595, p = 0.056)的唯一显著因素。结论:T1-ACs术后生存率高;然而,约20%的患者会复发。淋巴结转移仍然是影响长期生存的最重要因素。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Outcomes and recurrence patterns following resection of T1 ampullary carcinomas: single centre experience of 92 cases
Background
Resected early-stage (T1) ampullary carcinomas (ACs) have the best overall survival (OS) but can have higher postoperative morbidity compared to higher-stage ACs and other periampullary cancers.
Method
A retrospective analysis of resected T1-ACs at Tata Memorial Centre, Mumbai, from January 2012 to December 2022 was performed. Perioperative and long-term outcomes were assessed.
Results
A total of 92 patients underwent resection for T1-ACs, with a significant morbidity rate (Clavien-Dindo ≥3) of 38%, and a clinically relevant postoperative pancreatic fistula rate of 22.5%. The node positivity rate in resected T1-ACs was 25%. The 3- and 5-year OS rates were 77.9% and 74.5%, while recurrence-free survival (RFS) rates were 81.8% and 78.4%, respectively. There were 18 (19.6%) recurrences (2 local, 16 distant) during a median follow-up of 66.7 months. The 3- and 5-year OS after recurrence was 29.6% and 14.8% respectively. Lymph node metastasis was the sole significant factor affecting OS (HR 2.815, 95% CI: 1.114–7.112, p = 0.029) and RFS (HR 2.54, 95% CI: 0.978–6.595, p = 0.056).
Conclusion
T1-ACs have excellent survival after resection; however, about 20% of patients develop recurrence. Lymph node metastasis remains the most important factor affecting long-term survival.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Hpb
GASTROENTEROLOGY & HEPATOLOGY-SURGERY
CiteScore
5.60
自引率
3.40%
发文量
244
审稿时长
57 days
期刊介绍:
HPB is an international forum for clinical, scientific and educational communication.
Twelve issues a year bring the reader leading articles, expert reviews, original articles, images, editorials, and reader correspondence encompassing all aspects of benign and malignant hepatobiliary disease and its management. HPB features relevant aspects of clinical and translational research and practice.
Specific areas of interest include HPB diseases encountered globally by clinical practitioners in this specialist field of gastrointestinal surgery. The journal addresses the challenges faced in the management of cancer involving the liver, biliary system and pancreas. While surgical oncology represents a large part of HPB practice, submission of manuscripts relating to liver and pancreas transplantation, the treatment of benign conditions such as acute and chronic pancreatitis, and those relating to hepatobiliary infection and inflammation are also welcomed. There will be a focus on developing a multidisciplinary approach to diagnosis and treatment with endoscopic and laparoscopic approaches, radiological interventions and surgical techniques being strongly represented. HPB welcomes submission of manuscripts in all these areas and in scientific focused research that has clear clinical relevance to HPB surgical practice.
HPB aims to help its readers - surgeons, physicians, radiologists and basic scientists - to develop their knowledge and practice. HPB will be of interest to specialists involved in the management of hepatobiliary and pancreatic disease however will also inform those working in related fields.
Abstracted and Indexed in:
MEDLINE®
EMBASE
PubMed
Science Citation Index Expanded
Academic Search (EBSCO)
HPB is owned by the International Hepato-Pancreato-Biliary Association (IHPBA) and is also the official Journal of the American Hepato-Pancreato-Biliary Association (AHPBA), the Asian-Pacific Hepato Pancreatic Biliary Association (A-PHPBA) and the European-African Hepato-Pancreatic Biliary Association (E-AHPBA).
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


