二肽基肽酶-4抑制剂治疗2型糖尿病患者的心血管事件和心力衰竭:一项荟萃分析
IF 1.5
Q3 MEDICINE, RESEARCH & EXPERIMENTAL
Current Therapeutic Research-clinical and Experimental
Pub Date : 2025-01-01
DOI:10.1016/j.curtheres.2025.100804
引用次数: 0
摘要
背景2型糖尿病(T2DM)的全球患病率持续上升,患者面临心血管并发症,特别是心力衰竭(HF)的风险显著升高。目的:本研究旨在系统地检查二肽基肽酶4 (DPP-4)抑制剂使用者与非使用者的心血管后遗症,特别是心力衰竭。方法使用特定术语对scochrane、Embase和PubMed数据库进行检索,这些数据库比较了2型糖尿病(T2DM)患者使用DPP-4抑制剂和报告的心血管结局和心力衰竭事件。满足以下纳入标准的研究被纳入:比较T2DM患者使用DPP-4抑制剂的随机试验;研究持续时间大于24周;他们报告了心血管结局作为主要或次要终点。使用Stata 15mp (StataCorp LLC, College Station, Texas, USA)分析数据,使用95% ci的优势比(or)来表示结果。结果共纳入T2DM患者79,010例。共有37,895名患者被分配到DPP-4抑制剂组,而41,115名患者被分配到对照组。分析结果显示,在24至302周的平均随访期间,接受DPP-4抑制剂治疗的T2DM患者与未接受DPP-4抑制剂治疗的T2DM患者的心力衰竭发生率无显著差异(OR = 1.06;95% ci, 0.96-1.18;P = 0.452)。主要不良心血管事件(包括非致死性心肌梗死、非致死性卒中和心血管性死亡);Or = 1.01;95% ci, 0.95-1.08;P = 0.354),中风(OR = 1.01;95% ci, 0.78-1.30;P = 0.968),心肌梗死(OR = 0.89;95% ci, 0.73-1.07;P = 0.49),全因死亡率(OR = 1.03;95% ci, 0.96-1.11;P = 0.309)。结论:本分析显示,DPP-4抑制剂治疗并没有显著增加这些T2DM患者的心血管结局和心力衰竭,表明这些药物在心血管事件方面可能是安全的。本文章由计算机程序翻译,如有差异,请以英文原文为准。
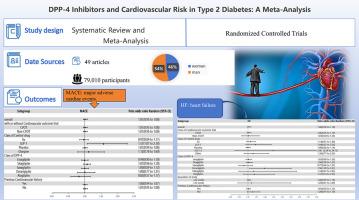
Cardiovascular Events and Heart Failure in Patients With Type 2 Diabetes Treated With Dipeptidyl Peptidase-4 Inhibitors: A Meta-Analysis
Background
The global prevalence of type 2 diabetes mellitus (T2DM) continues to rise, with patients facing significantly elevated risks of cardiovascular complications, particularly heart failure (HF).
Objective
This examination sought to methodically examine cardiovascular sequelae, notably heart failure, among users of dipeptidyl peptidase 4 (DPP-4) inhibitors when compared with nonusers.
Methods
Cochrane, Embase, and PubMed databases, which compared the use of DPP-4 inhibitors and reported cardiovascular outcomes and heart failure events in patients with type 2 diabetes mellitus (T2DM), were searched using specific terms. Studies were included if they satisfied the following inclusion criteria: they were randomized trials comparing DPP-4 inhibitor use in patients with T2DM; study duration was longer than 24 weeks; and they reported cardiovascular outcomes as their main or secondary end points. Stata 15 MP (StataCorp LLC, College Station, Texas, USA) was used to analyze the data, and odds ratios (ORs) with 95% CIs were used to represent the results.
Results
A total of 79,010 participants with T2DM were included. A total of 37,895 patients were assigned to the DPP-4 inhibitor group, whereas 41,115 patients were assigned to the control group. Results of the analysis showed that during a mean follow-up period ranging from 24 to 302 weeks, heart failure incidence did not differ significantly between T2DM patients treated with DPP-4 inhibitors and those who were not (OR = 1.06; 95% CI, 0.96–1.18; P = 0.452). Major adverse cardiovascular events (including nonfatal myocardial infarction, nonfatal stroke, and cardiovascular death; OR = 1.01; 95% CI, 0.95–1.08; P = 0.354), stroke (OR = 1.01; 95% CI, 0.78–1.30; P = 0.968), myocardial infarction (OR = 0.89; 95% CI, 0.73–1.07; P = 0.49), and all-cause mortality (OR = 1.03; 95% CI, 0.96–1.11; P = 0.309) were also similarly manifested in both groups.
Conclusions
The present analysis showed that treatment with DPP-4 inhibitors did not significantly increase cardiovascular outcomes and heart failure in these patients with T2DM, indicating that these drugs may be safe to use in terms of cardiovascular events.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
3.50
自引率
0.00%
发文量
31
审稿时长
3 months
期刊介绍:
We also encourage the submission of manuscripts presenting preclinical and very preliminary research that may stimulate further investigation of potentially relevant findings, as well as in-depth review articles on specific therapies or disease states, and applied health delivery or pharmacoeconomics.
CTR encourages and supports the submission of manuscripts describing:
• Interventions designed to understand or improve human health, disease treatment or disease prevention;
• Studies that focus on problems that are uncommon in resource-rich countries;
• Research that is "under-published" because of limited access to monetary resources such as English language support and Open Access fees (CTR offers deeply discounted English language editing);
• Republication of articles previously published in non-English journals (eg, evidence-based guidelines) which could be useful if translated into English;
• Preclinical and clinical product development studies that are not pursued for further investigation based upon early phase results.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


