超弧立体定向放疗治疗肺癌脑转移的疗效和安全性评价。
摘要
本研究评估了48例肺癌脑转移(LCBM)患者使用超弧度(HA)立体定向放疗(SRT)的疗效和安全性,同时确定了症状性脑放射性坏死(sCRN)的预后因素和高危预测因素。我们于2021年2月至2025年2月在江苏大学附属人民医院招募了48例诊断为LCBM的患者,其中44例为SRT组,4例为WBRT-boost组。收集临床资料,所有患者均行羟基磷灰石立体定向放疗。WBRT-boost组还获得了局部HA增强。处方剂量为24- 30gy,分3-5次,每周5次,根据病变特征进行治疗。我们评估了HA治疗LCBM的有效性和安全性。整个队列的1年总生存率(OS)、颅内远端无进展生存率(iDPFS)和颅内局部无进展生存率(iLPFS)分别为76.1、64.5和69.4%。对于野外远处转移,累积颅内客观缓解率(icORR)和颅内疾病控制率(icDCR)分别为52.1和64.6%,而野内转移为81.2和97.9%。WBRT-boost组的中位生存期为6.6个月,而SRT组的1年预后更好(生存期:79.1%;iDPFS: 67.0%;iLPFS: 71.8%)。与WBRT-boost相比,SRT表现出更好的局部控制(iLPFS, P = 0.044)和总生存(OS, P = 0.036),但远端控制(iDPFS, P = 0.086)无显著差异。多因素分析发现V12 bb0 10cc (HR 12.52, P = 0.011)和女性性别(HR 11.66, P = 0.026)是独立的预后因素。有症状的放射坏死12例(27.3%)均发生在SRT组。Logistic回归显示,较高的BED3 (HR 57.0, P = 0.009)独立增加了sCRN风险,而靶向治疗(HR 0.08, P = 0.024)显著降低了sCRN风险。基于hyperarc的立体定向分割放疗治疗肺癌脑转移安全可行,实现了有效的颅内肿瘤控制。与WBRT + boost相比,尽管需要仔细监测症状性放射性坏死,但SRT的治疗效果更好。进一步的调查应检查结合靶向药物和优化剂量分配的联合方法。
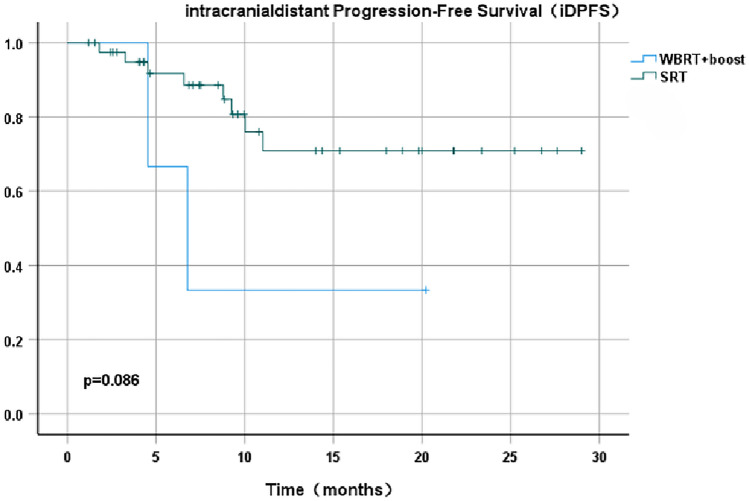
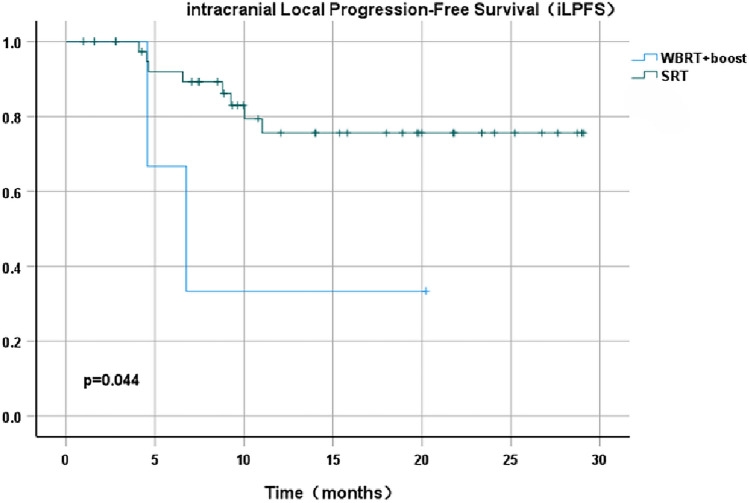
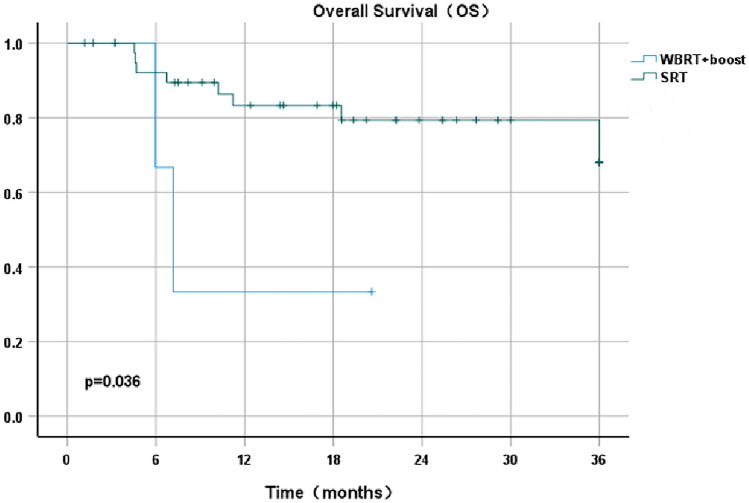
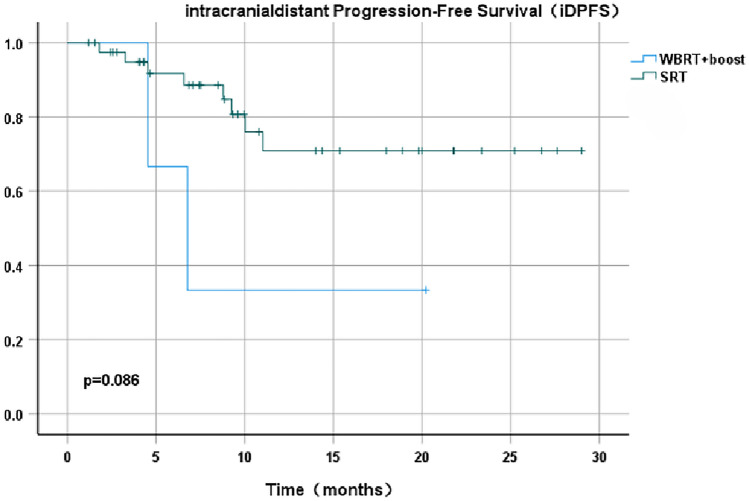
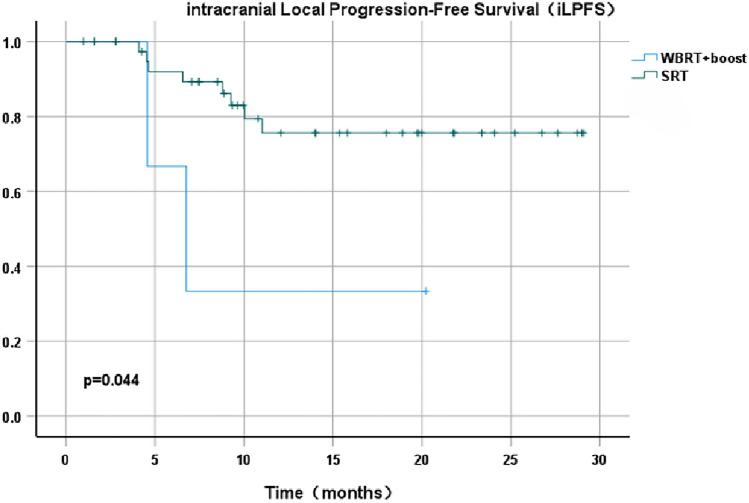
This study assessed the efficacy and safety of HyperArc (HA) stereotactic radiotherapy (SRT) in 48 patients with lung cancer brain metastases (LCBM) while identifying prognostic factors and high-risk predictors for symptomatic cerebral radiation necrosis (sCRN). We enrolled 48 patients diagnosed with LCBM at the People's Hospital Affiliated to Jiangsu University between February 2021 and February 2025, assigning 44 to the SRT group and 4 to the WBRT-boost group. Clinical data were collected, and all patients underwent HA stereotactic radiotherapy. The WBRT-boost group additionally received a local HA boost. Prescription doses of 24-30 Gy were administered in 3-5 fractions at 5 fractions weekly, tailored to lesion characteristics. We evaluated both the efficacy and safety of HA treatment for LCBM. The 1-year overall survival (OS), intracranial distant progression-free survival (iDPFS), and intracranial local progression-free survival (iLPFS) rates for the entire cohort were 76.1, 64.5, and 69.4%, respectively. For out-of-field distant metastases, the cumulative intracranial objective response rate (icORR) and intracranial disease control rate (icDCR) reached 52.1 and 64.6%, compared with 81.2 and 97.9% for in-field metastases. The WBRT-boost group exhibited a median OS of 6.6 months, while the SRT group achieved superior 1-year outcomes (OS:79.1%; iDPFS:67.0%; iLPFS:71.8%). Compared with WBRT-boost, SRT showed significantly better local control (iLPFS, P = 0.044) and overall survival (OS, P = 0.036), though distant control (iDPFS, P = 0.086) did not differ significantly. Multivariate analysis identified V12 > 10 cc (HR 12.52, P = 0.011) and female sex (HR 11.66, P = 0.026) as independent prognostic factors. All 12 symptomatic radiation necrosis cases (27.3%) occurred in the SRT group. Logistic regression demonstrated that higher BED3 (HR 57.0, P = 0.009) independently increased sCRN risk, whereas targeted therapy (HR 0.08, P = 0.024) significantly reduced it. HyperArc-based fractionated stereotactic radiotherapy proves safe and feasible for managing brain metastases from lung cancer, achieving effective intracranial tumor control. Compared with WBRT + boost, SRT yields superior therapeutic outcomes despite requiring careful monitoring for symptomatic radiation necrosis. Further investigations should examine combined approaches incorporating targeted agents and optimized dose distribution.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


