mPFC-rTMS对慢性失眠的影响:一项随机、双盲、安慰剂对照研究
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
背景内侧前额叶皮层(mPFC)可能在失眠的病理生理机制中发挥重要作用,可能是治疗失眠的潜在靶点。在此,我们旨在探讨重复经颅磁刺激(rTMS)治疗慢性失眠的有效性和安全性。方法采用先导、双盲、随机、假对照试验。研究人员招募了62名患有慢性失眠症的参与者,并将他们随机分配到主动或假性经颅磁刺激组。41名患者完成了针对mPFC的20次积极或虚假干预,并在基线、干预结束和随访时进行了评估。结果干预4周后,治疗组的有效率(51.7%)和缓解率(44.8%)显著高于治疗组(20.8%)和缓解率(16.7%),p = 0.037和p = 0.048。随访4周,两组有效率和缓解率无显著差异。使用匹兹堡睡眠质量指数(PSQI)、睡眠发作潜伏期、日常干扰和催眠药物使用的失眠严重程度在组和时间之间存在显著的相互作用。事后分析显示,与假手术组相比,在4周干预结束时,活跃组的失眠症状(除总睡眠时间和睡眠效率外)有显著改善,在4周随访时,PSQI评分、睡眠发作潜伏期、睡眠效率、日常干扰和催眠药物使用均有显著改善。两组不良事件发生率比较,差异无统计学意义,治疗过程中均未发生严重不良事件。结论mpfc - rtms治疗慢性失眠症是一种安全有效的治疗方法。本文章由计算机程序翻译,如有差异,请以英文原文为准。
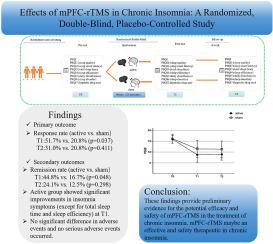
Effects of mPFC-rTMS in chronic Insomnia: A randomized, double-blind, placebo-controlled study
Background
Medial prefrontal cortex (mPFC) may play an important role in the pathophysiological mechanism of insomnia and may be a potential target for treating insomnia. Herein, we aimed to investigate the efficacy and safety of repetitive transcranial magnetic stimulation (rTMS) for chronic insomnia.
Methods
We conducted a pilot, double-blind, randomized, sham-controlled trial. 62 participants with chronic insomnia were recruited and randomly allocated to either the active or sham rTMS group. Forty-one patients completed 20 sessions of active or sham intervention targeting the mPFC and assessments at baseline, end of intervention, and follow-up.
Results
After 4-week intervention, the response rate and remission rate were significantly higher in the active group (51.7 % and 44.8 %) than those in the sham group (20.8 % and 16.7 %), with p = 0.037 and p = 0.048, respectively. At 4-week follow-up, the response rate and remission rate were not different between groups. There were significant interaction between group and time for insomnia severity using Pittsburgh Sleep Quality Index (PSQI) and sleep onset latency, daily disturbances, and hypnotic drug use. Post hoc analysis revealed that, compared with the sham group, the active group showed significant improvements in insomnia symptoms (except for total sleep time and sleep efficiency) at the end of the 4-week intervention, and significant improvements in PSQI scores, sleep onset latency, sleep efficiency, daily disturbances and hypnotic drug use at the 4-week follow-up. There were no statistically significant difference in adverse events between the two groups, and there were no serious adverse events occurred during treatment.
Conclusion
mPFC-rTMS maybe an effective and safety therapeutic in chronic insomnia.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


