美国军人处方药与睡眠时间、失眠和睡眠呼吸暂停之间的关系
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
研究目的:本研究探讨了处方药物与睡眠时间、失眠和睡眠呼吸暂停(SA)之间的关系。方法20,819名现役军人填写睡眠、人口统计学和生活方式特征问卷,并在问卷填写前6个月查阅其药房和医疗记录。按照美国医院处方系统药理学-治疗分类系统(PTCS)代码对FPMs进行分类,并在≥7、5-6和≤4小时的睡眠时间以及诊断为失眠和SA的患者和未诊断为失眠和SA的患者之间进行比较。结果在调整人口统计学和生活方式特征后,5-6小时和≤4小时的患者发生FPM的几率分别是报告≥7小时的SMs患者的1.19倍(95%可信区间[95% CI] = 1.12-1.27)和1.69倍(95% CI = 1.45-1.97)。与报告睡眠≥7小时的SMs相比,报告5-6小时的SMs在20个PTCS编码中的10个(特别是电解质/热量/水平衡药物)中有更高的FPMs调整几率,报告≤4小时的SMs在20个PTCS编码中的13个(特别是心血管和中枢神经系统(CNS)药物)中有更高的几率。与没有失眠或SA的SMs相比,失眠或SA的SMs发生FPM的调整几率分别高8.66 (95% CI = 5.89-12.71)和3.46 (95% CI = 2.90-4.12)。与没有这些诊断的SMs相比,患有失眠或SA的SMs在20个PTCS代码中的16个和18个中有更高的FPMs调整几率。心血管和中枢神经系统药物在两组睡眠障碍患者中最为普遍。结论随着睡眠时间的减少,许多不同类别药物的配药量增加,其中诊断为失眠或SA的SMs的配药量更高。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Associations between prescription medications and sleep duration, insomnia, and sleep apnea in US military service members
Study objectives
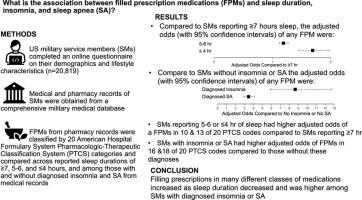
This study examined associations between filled prescription medications (FPMs) and sleep duration, insomnia, and sleep apnea (SA).
Methods
Active-duty service members (SMs) (n = 20,819) completed a questionnaire on sleep, demographics, and lifestyle characteristics and permitted access to their pharmacy and medical records 6-months before questionnaire completion. FPMs were classified by American Hospital Formulary System Pharmacologic-Therapeutic Classification System (PTCS) codes and compared across sleep durations of ≥7, 5–6, and ≤4 h and among those with and without diagnosed insomnia and SA.
Results
Compared to SMs reporting ≥7 h sleep, those reporting 5–6 and ≤4 h had 1.19 (95 %confidence interval [95 %CI] = 1.12–1.27) and 1.69 (95 %CI = 1.45–1.97) times higher odds of a FPM, respectively, after adjustment for demographics and lifestyle characteristics. Compared to SMs reporting ≥7 h sleep, those reporting 5–6 h had higher adjusted odds of FPMs in 10 of 20 PTCS codes--particularly electrolyte/caloric/water-balance agents--and those reporting ≤4 h had higher odds in 13 of 20 PTCS codes--particularly cardiovascular and central nervous system (CNS) agents. SMs with insomnia or SA had 8.66 (95 %CI = 5.89–12.71) and 3.46 (95 %CI = 2.90–4.12) higher adjusted odds of an FPM compared to those without insomnia or SA, respectively. SMs with insomnia or SA had higher adjusted odds of FPMs in 16 and 18 of 20 PTCS codes compared to those without these diagnoses. Cardiovascular and CNS agents were most prevalent in both sleep-disordered groups.
Conclusion
Filling prescriptions in many different classes of medications increased as sleep duration decreased and was higher among SMs with diagnosed insomnia or SA.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


