比较胱抑素C估计GFR与肌酐估计GFR在急性肾损伤恢复中的作用
IF 5.7
2区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
摘要
目前的指南推荐基于肌酐估计肾小球滤过率(eGFRcr)来评估急性肾损伤(AKI)后肾脏恢复情况;然而,由于肌肉量的减少,这可能是不准确的。基于胱抑素c的eGFR (eGFRcys)是一种不受类似影响的替代方案。此外,结合eGFRcr和eGFRcys差异的简单计算(如肌酐肌指数,CMI)可能提示预后。我们试图确定AKI后eGFRcr是否与eGFRcys不同,以及CMI是否与死亡率相关。方法德比地区AKI风险(ARID)研究是一项前瞻性平行组队列研究。有和没有暴露于AKI的住院参与者在年龄、基线肾功能和糖尿病方面按1:1匹配。比较849名参与者入院后3个月的eGFRcr和eGFRcys。在5年时评估CMI与包括死亡率、心力衰竭和住院治疗在内的预后之间的关系。结果segfrcys低于eGFRcr(53.4,[四分位数间距,IQR: 34.3-85.5] vs. 68.4 [IQR: 52.5-84.7] ml/min / 1.73 m2, P <;0.001), AKI患者差异更显著。eGFRcr对慢性肾脏疾病(CKD)患者的分类更多(AKI组:eGFRcr <;60 ml/min / 1.73 m2占44.9%;eGFRcys & lt;60毫升/分钟每1.73平方米69.6%,P <;0.001)。在AKI组中,较高的CMI与较低的5年死亡率独立相关(校正风险比:0.931 [0.874-0.992]mg/d / 1.73 m2, P = 0.03)。结论:AKI后3个月,肌酐与胱抑素c测定的eGFR存在显著差异,两者之间差异的大小与随后的死亡率有关。需要进一步的研究来确定AKI后患者评估的最佳方法。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Comparing Cystatin C Estimated GFR With Creatinine Estimated GFR in Acute Kidney Injury Recovery
Introduction
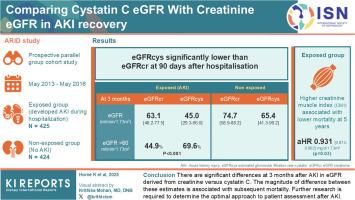
Current guidelines recommend creatinine-based estimated glomerular filtration rate (eGFRcr) to assess kidney recovery after acute kidney injury (AKI); however, this may be inaccurate because of loss of muscle mass. Cystatin C-based eGFR (eGFRcys) is an alternative that is not similarly affected. In addition, simple calculations (e.g., creatinine muscle index, CMI) incorporating the difference between eGFRcr and eGFRcys may indicate prognosis. We sought to determine whether eGFRcr differs from eGFRcys after AKI and whether CMI is associated with mortality.
Methods
The AKI Risk in Derby (ARID) study is a prospective parallel-group cohort study. Hospitalized participants with and without exposure to AKI were matched 1:1 for age, baseline kidney function, and diabetes. eGFRcr and eGFRcys at 3 months after admission were compared in 849 participants. Associations between CMI and outcomes, including mortality, heart failure, and hospitalization were assessed at 5 years.
Results
eGFRcys was lower than eGFRcr (53.4, [interquartile range, IQR: 34.3–85.5] vs. 68.4 [IQR: 52.5–84.7] ml/min per 1.73 m2, P < 0.001), with more pronounced differences in those with AKI. eGFRcys categorized more participants with chronic kidney disease (CKD) (in AKI group: eGFRcr < 60 ml/min per 1.73 m2 in 44.9%; eGFRcys < 60 ml/min per 1.73 m2 in 69.6%, P < 0.001). In the AKI group, higher CMI was independently associated with lower mortality at 5 years (adjusted hazard ratio: 0.931 [0.874–0.992] mg/d per 1.73 m2, P = 0.03).
Conclusion
There are significant differences at 3 months after AKI in eGFR derived from creatinine versus cystatin C. The magnitude of difference between these estimates is associated with subsequent mortality. Further research is required to determine the optimal approach to patient assessment after AKI.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Kidney International Reports
Medicine-Nephrology
CiteScore
7.70
自引率
3.30%
发文量
1578
审稿时长
8 weeks
期刊介绍:
Kidney International Reports, an official journal of the International Society of Nephrology, is a peer-reviewed, open access journal devoted to the publication of leading research and developments related to kidney disease. With the primary aim of contributing to improved care of patients with kidney disease, the journal will publish original clinical and select translational articles and educational content related to the pathogenesis, evaluation and management of acute and chronic kidney disease, end stage renal disease (including transplantation), acid-base, fluid and electrolyte disturbances and hypertension. Of particular interest are submissions related to clinical trials, epidemiology, systematic reviews (including meta-analyses) and outcomes research. The journal will also provide a platform for wider dissemination of national and regional guidelines as well as consensus meeting reports.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


