澳大利亚和奥特罗阿/新西兰的首次癫痫发作护理:处理癫痫部门间全球行动计划的保健服务需求
IF 2.3
3区 医学
Q2 BEHAVIORAL SCIENCES
引用次数: 0
摘要
目的探讨澳大利亚和新西兰(新西兰)首次癫痫发作诊所(FSCs)的现状,并根据癫痫和其他神经系统疾病跨部门全球行动计划(IGAP)确定影响患者获得这些服务的可改变的风险因素。方法对澳大利亚癫痫学会(ESA)的神经科医生、癫痫科医生和单位负责人进行在线调查。其他未被调查的诊所通过专业网络和个人沟通确定。使用研究电子数据采集(REDCap)软件记录调查结果。结果调查结果确定了澳大利亚和新西兰的24个首次癫痫发作诊所,包括21个成人和3个儿科服务。这些服务包括23个大都会服务和1个区域服务;15个是专门的fsc。在17项服务中,区域患者占患者基数的20% %以上。21家(88 %)服务机构利用了远程医疗,8家(33 %)服务机构通过远程医疗为半数以上的患者看病。FSC初次预约的中位数估计等待时间为6 周(IQR 3-15,范围2-56)。只有20% %的服务由临床护士/护理协调员提供支持。这是最常见的服务需求(58% %的服务)。还注意到需要增加高级医务人员(占服务的54% %)和初级医务人员(45% %)。最常报告的获取障碍包括诊所能力有限、人员不足、转诊不当、患者不出席以及调查延误。意义:在澳大利亚和新西兰,成人首次癫痫发作服务已经建立。尽管服务广泛覆盖大都市,但在澳大利亚和奥特罗阿/新西兰的区域地区仍然缺乏首次发作诊所,并且在现有服务中需要增加护理和医务人员。这项研究表明,在哪些方面的改进可能会导致澳大利亚和新西兰更好地获得首次癫痫发作护理,并实现IGAP的目标。本文章由计算机程序翻译,如有差异,请以英文原文为准。
First seizure care in Australia and Aotearoa/New Zealand: health service needs for addressing the intersectoral global action plan in epilepsy
Objective
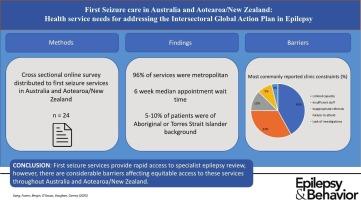
To explore the current state of first seizure clinics (FSCs) in Australia and Aotearoa/New Zealand (NZ) and identify modifiable risk factors impacting patient access to these services in line with the Intersectoral Global Action Plan on Epilepsy and Other Neurological Disorders (IGAP).
Methods
An online survey was distributed to neurologists, epileptologists and heads-of-unit affiliated with the Epilepsy Society of Australia (ESA). Additional clinics not captured by the survey were identified through professional networks and personal communication. Survey responses were recorded using Research Electronic Data Capture (REDCap) software.
Results
Survey responses identified 24 first seizure clinics across Australia and Aotearoa/NZ, including 21 adult and 3 paediatric services. These comprised 23 metropolitan services and 1 regional service; 15 were dedicated FSCs. Regional patients comprised more than 20 % of the patient base in 17 services. Telehealth was utilized by 21 (88 %) services, with 8 (33 %) services seeing over half their patients via telehealth. Median estimated wait time for initial FSC appointment was 6 weeks (IQR 3–15, range 2–56). Only 20 % of services were supported by a clinical nurse/care coordinator. This was the most commonly reported service need (58 % of services). Need for additional senior medical staff (54 % of services) and junior medical staff (45 %) was also noted. The most frequently reported barriers to access included limited clinic capacity, insufficient staffing, inappropriate referrals, patients’ failure to attend and delays to investigations.
Significance
First seizure services for adults are well established across Australia and Aotearoa/NZ. Despite broad metropolitan coverage in services, there remains a lack of first seizure clinics in regional areas of Australia and Aotearoa/NZ, and a need for additional nursing and medical staff in established services. This study demonstrates areas where improvements could potentially lead to better access to first seizure care across Australia and Aotearoa/NZ and achieve the goals of the IGAP.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Epilepsy & Behavior
医学-行为科学
CiteScore
5.40
自引率
15.40%
发文量
385
审稿时长
43 days
期刊介绍:
Epilepsy & Behavior is the fastest-growing international journal uniquely devoted to the rapid dissemination of the most current information available on the behavioral aspects of seizures and epilepsy.
Epilepsy & Behavior presents original peer-reviewed articles based on laboratory and clinical research. Topics are drawn from a variety of fields, including clinical neurology, neurosurgery, neuropsychiatry, neuropsychology, neurophysiology, neuropharmacology, and neuroimaging.
From September 2012 Epilepsy & Behavior stopped accepting Case Reports for publication in the journal. From this date authors who submit to Epilepsy & Behavior will be offered a transfer or asked to resubmit their Case Reports to its new sister journal, Epilepsy & Behavior Case Reports.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


