家族性乳糜微粒血症综合征的神经变性。
IF 4.6
3区 医学
Q2 PHARMACOLOGY & PHARMACY
引用次数: 0
摘要
背景和目的:家族性乳糜小元素血症综合征(FCS)是一种罕见的常染色体隐性遗传病,与甘油三酯浓度显著升高和急性胰腺炎相关,但神经性疼痛和认知功能障碍也越来越被认识到。本研究对FCS患者的躯体和自主神经病变进行了详细的量化。方法:16名FCS患者和16名年龄和性别匹配的对照组接受了脂质谱、神经病变症状和残疾、振动感知、角膜共聚焦显微镜(CCM)和心脏自主反射测试的评估。结果:FCS患者的年龄(36.4 [26.5-47.2]vs 36.7[31.3-46.9]岁,P = 0.7)、性别分布(男性44% [n = 7] vs 50% [n = 8], P = 0.7)、体重指数(23.7 [20.3-27.1]vs 24.7 [22.3-27.2] kg/m2, P = 0.5)、糖化血红蛋白(36.0 [32.5-39.2]vs 36.8 [33.0-38.0] mmol/mol, P = 0.9)具有可比性。FCS患者的甘油三酯显著升高(23.7 [17.4-34.8]vs 1.0 [0.7-1.3] mmol/L, P < .001),而低密度脂蛋白胆固醇(0.9 [0.7-1.2]vs 2.7 [2.3-3.1] mmol/L, P < .001)和高密度脂蛋白胆固醇(0.4 [0.3-0.6]vs 1.5 [1.3-1.9] mmol/L, P < .001)较低。神经病变症状谱评分(4 [0-14]vs 0, P = 0.003)、神经病变功能障碍评分(1 [0-3.5]vs 0, P = 0.01)、振动感知阈值(6.5 [4.7-8.1]vs 3.0[2.0-3.5]伏,P < 0.001)均较高,角膜神经纤维密度(30.2 [27.3-32.3]vs 37.0[32.5-38.5])均较高。/mm2, P < 0.001),角膜神经分支密度(54.1 [42.0 ~ 76.6]vs 100.5 [67.0 ~ 147.1];/mm2, P < 0.001)、角膜神经纤维长度(20.0 [18.3-25.5]vs 27.5 [23.9-34.3] mm/mm2, P < 0.001)、深呼吸心率变异性(17.0 [14.2-28.0]vs 29.5[25.2-34.7]次/分,P = 0.002)、呼气吸气比(1.18 [1.14-1.29]vs 1.36 [1.25-1.41], P = 0.001)均低于对照组。结论:FCS与神经病变症状、振动感知升高、小神经纤维损伤和心脏自主神经功能障碍有关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Neurodegeneration in familial chylomicronemia syndrome
BACKGROUND AND OBJECTIVES
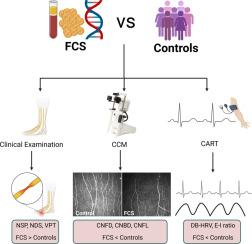
Familial chylomicronemia syndrome (FCS) is a rare autosomal recessive disorder associated with markedly elevated triglyceride concentration and acute pancreatitis, but neuropathic pain and cognitive dysfunction are also increasingly recognized. This study undertook detailed quantification of somatic and autonomic neuropathy in participants with FCS.
METHODS
Sixteen individuals with FCS and 16 age and sex-matched controls underwent assessment of the lipid profile, neuropathic symptoms and disability, vibration perception, corneal confocal microscopy (CCM), and cardiac autonomic reflex testing.
RESULTS
Age (36.4 [26.5-47.2] vs 36.7 [31.3-46.9] years, P = .7), gender distribution (males 44% [n = 7] vs 50% [n = 8], P = .7), body mass index (23.7 [20.3-27.1] vs 24.7 [22.3-27.2] kg/m2, P = .5), and glycosylated hemoglobin (36.0 [32.5-39.2] vs 36.8 [33.0-38.0] mmol/mol, P = .9) were comparable between participants with FCS and controls. Triglycerides were significantly higher (23.7 [17.4-34.8] vs 1.0 [0.7-1.3] mmol/L, P < .001), whilst low-density lipoprotein cholesterol (0.9 [0.7-1.2] vs 2.7 [2.3-3.1] mmol/L, P < .001) and high-density lipoprotein cholesterol (0.4 [0.3-0.6] vs 1.5 [1.3-1.9] mmol/L, P < .001) were lower in participants with FCS. The Neuropathy Symptom Profile Score (4 [0-14] vs 0, P = .003), Neuropathy Disability Score (1 [0-3.5] vs 0, P = .01), and vibration perception threshold (6.5 [4.7-8.1] vs 3.0 [2.0-3.5] volts, P < .001) were higher, whilst corneal nerve fiber density (30.2 [27.3-32.3] vs 37.0 [32.5-38.5] no./mm2, P < .001), corneal nerve branch density (54.1 [42.0-76.6] vs 100.5 [67.0-147.1] no./mm2, P < .001), corneal nerve fiber length (20.0 [18.3-25.5] vs 27.5 [23.9-34.3] mm/mm2, P < .001), deep breathing heart rate variability (17.0 [14.2-28.0] vs 29.5 [25.2-34.7] beats/min, P = .002), and expiration to inspiration ratio (1.18 [1.14-1.29] vs 1.36 [1.25-1.41], P = .001) were lower in participants with FCS compared to controls.
CONCLUSION
FCS is associated with neuropathic symptoms, elevated vibration perception, small nerve fiber damage, and cardiac autonomic dysfunction.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
7.00
自引率
6.80%
发文量
209
审稿时长
49 days
期刊介绍:
Because the scope of clinical lipidology is broad, the topics addressed by the Journal are equally diverse. Typical articles explore lipidology as it is practiced in the treatment setting, recent developments in pharmacological research, reports of treatment and trials, case studies, the impact of lifestyle modification, and similar academic material of interest to the practitioner.
Sections of Journal of clinical lipidology will address pioneering studies and the clinicians who conduct them, case studies, ethical standards and conduct, professional guidance such as ATP and NCEP, editorial commentary, letters from readers, National Lipid Association (NLA) news and upcoming event information, as well as abstracts from the NLA annual scientific sessions and the scientific forums held by its chapters, when appropriate.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


