停用脂质调节剂和未能达到心血管危险人群的目标LDL胆固醇水平
IF 4.6
3区 医学
Q2 PHARMACOLOGY & PHARMACY
引用次数: 0
摘要
背景:低密度脂蛋白胆固醇(LDL-C)控制仍然不够理想,关于脂质调节剂(LMAs)依从性如何随动脉粥样硬化性心血管疾病(ASCVD)风险的变化而变化的证据有限。目的:探讨LDL-C水平、LMAs依从性和ASCVD风险之间的关系。方法:在2013年至2023年期间,处方LMAs的成年人(n = 4262)(中位年龄60岁,49%为男性)被分类为低(结果:所有风险组的平均LDL-C从3.6±1.1 mmol/L(139.2±42.5 mg/dL)降至2.7±1.1 mmol/L(104.4±42.5 mg/dL),只有23%的人达到结论:长期坚持LMAs仍然是一个挑战,特别是在低风险人群中。目标实现较差,突出了治疗优化、患者参与和监测方面的差距。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Discontinuation of lipid-modifying agents and failure to achieve target LDL cholesterol levels across cardiovascular risk groups
BACKGROUND
Low-density lipoprotein cholesterol (LDL-C) control remains suboptimal, with limited evidence on how adherence to lipid-modifying agents (LMAs) varies by atherosclerotic cardiovascular disease (ASCVD) risk.
OBJECTIVE
To examine the relationship between LDL-C levels, adherence to LMAs, and ASCVD risk.
METHODS
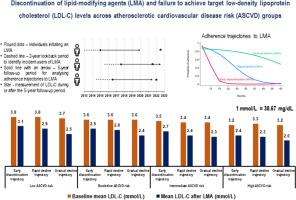
Adults (n = 4,262) prescribed LMAs between 2013 and 2023 (median age 60 years, 49% male) were categorized into low (<5%), borderline (5% to <7.5%), intermediate (7.5% to <20%), and high (≥20%) 10-year ASCVD risk groups. Adherence was defined as having ≥1 prescription of LMA every 6 months, with adherence trajectories identified over 5 years using group-based trajectory analysis: gradual decline, rapid decline, and early discontinuation.
RESULTS
Average LDL-C decreased from 3.6 ± 1.1 mmol/L (139.2 ± 42.5 mg/dL) to 2.7 ± 1.1 mmol/L (104.4 ± 42.5 mg/dL) across all risk groups, with only 23% achieving <1.8 mmol/L (69.6 mg/dL) and 18% achieving ≥50% reduction. LDL-C was highest in the early discontinuation trajectory, across all ASCVD risk groups, averaging 2.9 mmol/L (112.1 mg/dL) in the low ASCVD risk group (42%), 2.8 mmol/L (108.3 mg/dL) in the borderline (13%), 2.5 mmol/L (96.7 mg/dL) in the intermediate (33%), and 2.3 mmol/L (88.9 mg/dL) in the high-risk group (11%). Higher LDL-C was associated with younger age, being male, non-smoking status, absence of diabetes, untreated blood pressure, early LMA discontinuation, higher total cholesterol ratio, and lower high-density lipoprotein cholesterol.
CONCLUSION
Long-term adherence to LMAs remains a challenge, particularly in low-risk. Target achievement was poor, highlighting gaps in therapeutic optimization, patient engagement, and monitoring.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
7.00
自引率
6.80%
发文量
209
审稿时长
49 days
期刊介绍:
Because the scope of clinical lipidology is broad, the topics addressed by the Journal are equally diverse. Typical articles explore lipidology as it is practiced in the treatment setting, recent developments in pharmacological research, reports of treatment and trials, case studies, the impact of lifestyle modification, and similar academic material of interest to the practitioner.
Sections of Journal of clinical lipidology will address pioneering studies and the clinicians who conduct them, case studies, ethical standards and conduct, professional guidance such as ATP and NCEP, editorial commentary, letters from readers, National Lipid Association (NLA) news and upcoming event information, as well as abstracts from the NLA annual scientific sessions and the scientific forums held by its chapters, when appropriate.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


