依从西班牙共识关于哮喘患者减少口服皮质类固醇使用建议的程度:一项基于问卷的观察性研究
Q4 Medicine
引用次数: 0
摘要
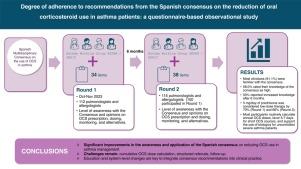
西班牙最近发表了关于减少口服皮质类固醇(OCS)在哮喘管理中的使用的共识,以解决该地区OCS过度使用的问题。本研究评估了卫生保健专业人员对这一共识的认识和实施程度。方法采用纵向研究方法,由肺科医师和变态反应科医师进行调查,每隔6个月进行2轮。关键指标包括OCS处方率、对建议的依从性和其他临床医生报告的做法。结果两轮研究分别有112名和115名参与者完成,其中过敏症专家和肺科专家的比例相等。大多数人(91.1%)熟悉共识,58.0%的人认为他们的知识很高。53%的人表示6个月后知识有所增长。关于OCS的剂量,第一轮70.5%和第二轮66.1%的人认为5mg /天的泼尼松是低剂量治疗。大多数常规计算OCS年剂量,使用数字工具进行剂量计算的情况显著增加。大多数临床医生倾向于5-7天的短期OCS疗程,并支持对未控制的严重哮喘患者使用生物制剂维持OCS。结论:这些发现表明,在西班牙共识发表后,OCS的使用显著减少,哮喘管理指南的依从性得到改善。反复的教育干预在改变处方行为和优化哮喘护理方面是有效的。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Degree of Adherence to Recommendations From the Spanish Consensus on the Reduction of Oral Corticosteroid Use in Asthma Patients: A Questionnaire-based Observational Study
Introduction
The Spanish consensus on the reduction of oral corticosteroid (OCS) use in asthma management was recently published to address the issue of OCS overuse in this area. This study evaluates the degree of awareness and implementation of this consensus by healthcare professionals.
Methods
A longitudinal study was conducted with a survey completed by pulmonologists and allergists in 2 rounds conducted 6 months apart. Key metrics included OCS prescribing rates, adherence to recommendations, and other clinician-reported practices.
Results
Both rounds were completed by 112 and 115 participants, respectively, with equal representation from allergists and pulmonologists. Most (91.1%) were familiar with the consensus, and 58.0% rated their knowledge as high. Fifty-three percent reported increased knowledge after 6 months. Regarding OCS dosing, 70.5% in the first round and 66.1% in the second round considered 5 mg/day of prednisone to be low-dose therapy. A majority routinely calculated annual OCS doses, with a notable rise in the use of digital tools for dose calculations. Most clinicians favored 5–7 days for short OCS courses and supported the use of biologics for patients with uncontrolled severe asthma on maintenance OCS.
Conclusions
These findings suggest a notable reduction in OCS use and improved adherence to asthma management guidelines following the publication of the Spanish consensus. Repeated educational interventions appear effective in modifying prescribing behaviors and optimizing asthma care.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Open Respiratory Archives
Medicine-Pulmonary and Respiratory Medicine
CiteScore
1.10
自引率
0.00%
发文量
58
审稿时长
51 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


