院前肾上腺素管理与院外接受体外心肺复苏的休克性心脏骤停患者短期预后的关系:倾向评分匹配分析
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
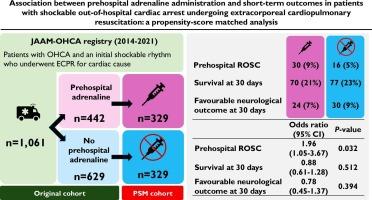
在院外心脏骤停(OHCA)和初始休克性心律患者进行体外复苏(ECPR)时,肾上腺素对神经系统预后的影响仍不确定。本研究旨在探讨院前肾上腺素与患者临床预后的关系。该多中心前瞻性研究(JAAM-OHCA注册)在2014年至2021年间纳入了81234例OHCA患者。因心脏原因接受ECPR的初始震荡性心律患者符合本研究的条件。30天的主要结果是良好的神经学结果。次要终点为院前自发循环恢复(ROSC)或30天生存率。进行倾向评分匹配分析以调整混杂因素并评估院前肾上腺素与研究结果之间的独立关联。结果1061例患者中442例(41.7%)接受院前肾上腺素治疗,619例(58.3%)未接受院前肾上腺素治疗。在329对配对患者中,肾上腺素组院前ROSC率显著高于肾上腺素组(30 [9%]vs 16 [5%]);校正优势比[OR] 1.96, 95%可信区间[CI] 1.05 ~ 3.67, P = 0.03)。然而,30天生存率(70 [21%]vs 77 [23%];调整OR 0.88, 95% CI 0.61-1.28, P = 0.51)和30天良好的神经预后(24 [7%]vs 30 [9%];校正OR 0.78, 95% CI 0.45-1.37, P = 0.39),差异无统计学意义。结论:在接受ECPR的OHCA和初始震荡节律患者中,院前肾上腺素与院前ROSC增加显著相关,但与生存期增加和30天良好的神经预后无关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Association between prehospital adrenaline administration and short-term outcomes in patients with shockable out-of-hospital cardiac arrest undergoing extracorporeal cardiopulmonary resuscitation: a propensity-score matched analysis
Background
In patients with out-of-hospital cardiac arrest (OHCA) and an initial shockable rhythm undergoing extracorporeal resuscitation (ECPR), the effect of adrenaline on neurological outcomes remains uncertain. This study aimed to investigate the association between prehospital adrenaline and clinical outcomes in this patient population.
Methods
This multicentre, prospective study (JAAM-OHCA registry) enrolled 81,234 patients with OHCA between 2014 and 2021. Patients with an initial shockable rhythm who underwent ECPR for a cardiac cause were eligible for this study. The primary outcome was a favourable neurological outcome at 30 days. The secondary outcome was prehospital return of spontaneous circulation (ROSC) or 30-day survival. A propensity score-matched analysis was performed to adjust for confounding and evaluate the independent association between prehospital adrenaline and study outcomes.
Results
Among 1,061 patients, 442 (41.7 %) received prehospital adrenaline and 619 (58.3 %) did not. In 329 matched pairs, the prehospital ROSC rate was significantly higher in the adrenaline group (30 [9 %] vs 16 [5 %]; adjusted odds ratio [OR] 1.96, 95 % confidence interval [CI] 1.05–3.67, P = 0.03). However, 30-day survival (70 [21 %] vs 77 [23 %]; adjusted OR 0.88, 95 % CI 0.61–1.28, P = 0.51) and a favourable neurological outcome at 30 days (24 [7 %] vs 30 [9 %]; adjusted OR 0.78, 95 % CI 0.45–1.37, P = 0.39) were not significantly different.
Conclusions
In patients with OHCA and an initial shockable rhythm who underwent ECPR, prehospital adrenaline was significantly associated with increased prehospital ROSC, but not with increased in survival and a favourable neurological outcome at 30 days.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


