pci后血管血流储备分数(vFFR)与光学相干断层扫描(OCT)结果的关系:FAST OCT研究结果
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
目的pci术后血流储备分数(FFR)降低和光学相干断层扫描(OCT)结果不理想与预后受损有关。血管造影衍生血管FFR (vFFR)已成为压力丝法FFR的精确替代品。本研究试图确定pci后vFFR与OCT结果之间的关系。方法与结果FAST OCT研究纳入200例非st段抬高急性冠状动脉综合征(NSTE-ACS)和中重度冠状动脉狭窄患者。pci后OCT和至少一条研究血管vFFR评估的患者被纳入pci后亚分析。完整的PCI后OCT和vFFR数据可获得109条血管(100例患者)。pci后vFFR中位数为0.93[25 - 75百分位数0.90-0.96],血管最小管腔面积中位数为3.48 mm2[25 - 75百分位数2.42-4.89],支架内MLA中位数为5.37[25 - 75百分位数4.14-6.82]。在多变量分析中,pci后vFFR与血管MLA显著相关(vFFR每降低0.10,平均降低20.6% (95% CI - 34.6%至- 3.7%),p = 0.021)。pci后vFFR检测MLA≤4.5 mm2的最佳临界值为0.92(敏感性60.5%,特异性87.9%)。近端vFFR梯度对近端残留病变的诊断性能较好(AUC为0.80),而支架内梯度对支架扩张不足的诊断性能较差(AUC为0.52)。结论svffr与MLA有显著相关性,vFFR≤0.92对MLA≤4.5 mm2有较好的特异性。pci后vFFR和节段梯度可能有助于识别次优MLA和近端疾病,但不能识别支架扩张不足。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Association between post-PCI vessel fractional flow reserve (vFFR) and optical coherence tomography (OCT) findings: Results from the FAST OCT study
Aims
Reduced post-PCI fractional flow reserve (FFR) and suboptimal optical coherence tomography (OCT) findings are associated with impaired outcomes. Angiography-derived vessel FFR (vFFR) has emerged as an accurate alternative to pressure-wire based FFR. This study sought to define the association between post-PCI vFFR and OCT findings.
Methods and results
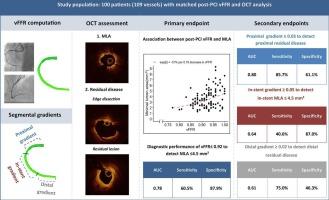
The FAST OCT study included 200 patients with non-ST-elevation acute coronary syndrome (NSTE-ACS) and intermediate to severe coronary artery stenosis. Patients with post-PCI OCT and vFFR evaluation of at least one study vessel were included in this post-PCI sub-analysis. Complete post PCI OCT and vFFR data were available for 109 vessels (100 patients). Median post-PCI vFFR was 0.93 [25th–75th percentile 0.90–0.96], median vessel minimal lumen area (MLA) was 3.48 mm2 [25th–75th percentile 2.42–4.89] and median in-stent MLA was 5.37 [25th–75th percentile 4.14–6.82]. In multivariable analysis, post-PCI vFFR was significantly associated with vessel MLA (average decrease of 20.6 % per 0.10 decrease in vFFR (95 % CI −34.6 % to −3.7 %), p = 0.021). The optimal cutoff value of post-PCI vFFR to detect an MLA ≤ 4.5 mm2 was 0.92 (sensitivity 60.5 %, specificity 87.9 %). The proximal vFFR gradient showed a good diagnostic performance to detect proximal residual disease (AUC 0.80), whereas the diagnostic performance of the in-stent gradient to detect stent underexpansion was poor (AUC 0.52).
Conclusions
vFFR was significantly associated with MLA and a vFFR ≤ 0.92 had a good specificity to detect an MLA ≤ 4.5 mm2. Post-PCI vFFR and segmental gradients may be of interest to identify suboptimal MLA’s and proximal disease, but could not identify stent underexpansion.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


