阻塞性睡眠呼吸暂停和阵发性心房颤动患者炎症和免疫激活的全身标志物。
IF 6.1
2区 医学
Q1 MEDICINE, GENERAL & INTERNAL
引用次数: 0
摘要
背景:心房颤动(AF)和阻塞性睡眠呼吸暂停(OSA)经常共存,可能通过共同的炎症途径增加心血管风险。炎症标志物在房颤和OSA患者中的具体作用尚不清楚。目的:本研究旨在确定阵发性房颤和OSA患者的炎症和免疫激活标志物是否升高,评估持续气道正压通气(CPAP)和肺静脉隔离(PVI)对这些标志物的影响,并评估它们与房颤复发和血栓栓塞风险等临床结局的相关性。方法:对143例阵发性房颤合并中重度OSA(呼吸暂停低通气指数≥15)患者进行研究。其中,99例随机分为CPAP加标准治疗组(n = 51)或单独标准治疗组(n = 48)。结果:OSA合并阵发性房颤患者的NGAL、PTX-3、GDF-15、MMP-9、VCAM1和ANGP2水平均高于健康对照组。这些指标与房颤和OSA严重程度相关性较差。CPAP对任何标志物均无改变作用。PTX3与房颤复发和血栓栓塞性卒中的高危评分相关。结论:中重度OSA和AF与炎症标志物升高相关。然而,CPAP治疗并没有显著影响这些水平。PTX-3可能对房颤复发和血栓栓塞风险具有预后价值。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Systemic markers of inflammation and immune activation in patients with obstructive sleep apnea and paroxysmal atrial fibrillation
Background
Atrial fibrillation (AF) and obstructive sleep apnea (OSA) frequently coexist, contributing to cardiovascular risk, possibly through shared inflammatory pathways. The specific role of inflammatory markers in patients with AF and OSA is not well established.
Aim
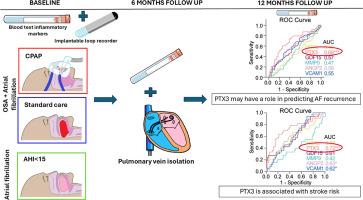
This study aimed to determine whether markers of inflammation and immune activation are elevated in patients with paroxysmal AF and OSA, assess the effects of continuous positive airway pressure (CPAP) and pulmonary vein isolation (PVI) on these markers, and evaluate their association with clinical outcomes, such as AF recurrence and thromboembolic risk.
Methods
We studied 143 patients with paroxysmal AF and moderate to severe OSA (apnea-hypopnea index ≥15). Of these, 99 were randomised to receive CPAP plus standard care (n = 51) or standard care alone (n = 48). A comparison group of 19 patients with paroxysmal AF and mild/no OSA (AHI <15) and 22 healthy controls were also included. Inflammatory markers related to leukocyte activation, vascular inflammation, and extracellular matrix remodelling were assessed at baseline, 6 months and 12 months follow-up.
Results
Patients with OSA and paroxysmal AF had higher levels of NGAL, PTX-3, GDF-15, MMP-9, VCAM1 and ANGP2 than healthy controls. These markers correlated poorly with AF and OSA severity. There was no modifying effect of CPAP on any marker. PTX3 was associated with AF recurrence and a high-risk score for thromboembolic stroke.
Conclusion
Moderate to severe OSA and AF are associated with elevated inflammatory markers. However, CPAP therapy did not significantly affect these levels. PTX-3 may hold prognostic value for AF recurrence and thromboembolic risk.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
9.60
自引率
6.20%
发文量
364
审稿时长
20 days
期刊介绍:
The European Journal of Internal Medicine serves as the official journal of the European Federation of Internal Medicine and is the primary scientific reference for European academic and non-academic internists. It is dedicated to advancing science and practice in internal medicine across Europe. The journal publishes original articles, editorials, reviews, internal medicine flashcards, and other relevant information in the field. Both translational medicine and clinical studies are emphasized. EJIM aspires to be a leading platform for excellent clinical studies, with a focus on enhancing the quality of healthcare in European hospitals.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


