克雷伯氏菌血流感染多药耐药现状、危险因素及对预后的影响来自前瞻性队列的见解。
IF 6.1
2区 医学
Q1 MEDICINE, GENERAL & INTERNAL
引用次数: 0
摘要
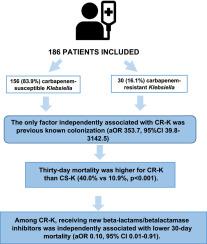
前言:我们旨在根据克雷伯氏菌对β -内酰胺的耐药情况描述其临床特征、危险因素和预后。材料和方法:单中心前瞻性队列研究,包括2021年1月至2023年12月期间首次发生克雷伯氏杆菌血症的所有成年患者。患者分为2组:克雷伯氏菌对碳青霉烯类敏感(CS-K);耐碳青霉烯克雷伯菌(CR-K)。预后的主要终点是30天死亡率。结果:186例患者中,156例(83.9%)为CS-K, 30例(16.1%)为CR-K。与CR-K独立相关的唯一因素是先前已知的定殖(aOR 353.7, 95% CI 39.8-3142.5)。CR-K组的30天死亡率高于CS-K组(40.0% vs 10.9%, p < 0.001)。CS-K组比CR-K组更频繁地使用适当的初始抗生素(75.6%比36.7%,p < 0.001)。在调整了可能的共同因素后,CR-K与较高的死亡率相关(aOR 3.97, 95% CI 1.40-9.12)。在CR-K患者中,接受新的β -内酰胺类/ β -内酰胺酶抑制剂与较低的30天死亡率独立相关(aOR 0.10, 95% CI 0.01-0.91)。这些患者的死亡率与碳青霉烯敏感克雷伯菌菌血症患者相似(10.9% vs 16.7%, p = 0.680)。结论:CR-K菌血症与较差的预后相关。先前的定植是与这种感染相关的最重要因素。在CR-K菌血症患者中使用活性新型β -内酰胺/ β -内酰胺酶抑制剂抗生素与更好的预后相关,与碳青霉烯敏感克雷伯菌菌株观察到的30天死亡率相匹配。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Current epidemiology, risk factors and influence on prognosis of multidrug resistance in Klebsiella spp. bloodstream infection. Insights from a prospective cohort
Introduction
We aimed to describe clinical characteristics, risk factors and prognosis in patients with Klebsiella spp. bacteremia according to their beta-lactam resistance profile.
Material and methods
Single-centre prospective cohort, including all adults patients with a first episode of Klebsiella spp. bacteriemia from January 2021 to December 2023. Patients were divided into 2 groups: Klebsiella spp. susceptible to carbapenems (CS-K)); and carbapenem-resistant Klebsiella spp. (CR-K). The primary endpoint for prognosis was 30-day mortality.
Results
Of the 186 patients included, 156 (83.9 %) were CS-K, and 30 (16.1 %) CR-K. The only factor independently associated with CR-K was previous known colonization (aOR 353.7, 95 %CI 39.8–3142.5). Thirty-day mortality was higher for CR-K than CS-K (40.0 % vs 10.9 %, p < 0.001). An adequate initial antibiotic was used more frequently in CS-K vs CR-K (75.6 % vs 36.7 %, p < 0.001). After adjusting for possible cofounding factors, CR-K was associated with higher mortality (aOR 3.97, 95 % CI 1.40–9.12). Among CR-K, receiving new beta-lactams/betalactamase inhibitors was independently associated with lower 30-day mortality (aOR 0.10, 95 % CI 0.01–0.91). Those patients had similar mortality than those with carbapenem-susceptible Klebsiella spp. bacteremia (10.9 % vs 16.7 %, p = 0.680)
Conclusions
CR-K bacteremia was associated with worse outcomes. Prior colonization was the most important factor associated with this infection. The use of active new betalactam/betalactamase inhibitor antibiotic in patients with CR-K bacteremia was associated with a better prognosis, matching the 30-day mortality observed in carbapenem-susceptible Klebsiella spp. strains.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
9.60
自引率
6.20%
发文量
364
审稿时长
20 days
期刊介绍:
The European Journal of Internal Medicine serves as the official journal of the European Federation of Internal Medicine and is the primary scientific reference for European academic and non-academic internists. It is dedicated to advancing science and practice in internal medicine across Europe. The journal publishes original articles, editorials, reviews, internal medicine flashcards, and other relevant information in the field. Both translational medicine and clinical studies are emphasized. EJIM aspires to be a leading platform for excellent clinical studies, with a focus on enhancing the quality of healthcare in European hospitals.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


