糖尿病营养治疗的进化范式:从碳水化合物计数到精确饮食
Q2 Medicine
引用次数: 0
摘要
全球糖尿病患病率呈上升趋势,需要先进的策略进行有效的管理。营养治疗在糖尿病治疗中起着至关重要的作用,有助于血糖控制、体重调节和并发症预防。历史上以碳水化合物计数和标准化膳食计划为中心,营养策略已经向更灵活、以患者为中心的方法发展。新出现的证据强调了根据患者的文化偏好、代谢特征和合并症进行个性化饮食干预的重要性。地中海饮食、停止高血压的饮食方法(DASH)和植物性饮食等方法已经证明对1型和2型糖尿病都有显著的益处。数字工具、行为科学以及营养基因组学和肠道微生物组的新见解的整合进一步支持了向精准营养的范式转变。在这篇评论中,我们强调了糖尿病护理中营养治疗的演变,强调了从通用推荐到个性化饮食策略的转变,旨在改善长期结果。它强调了精准营养在优化血糖控制、减轻并发症和提高患者依从性方面的潜力。我们认为,糖尿病护理的未来取决于个性化的营养模式,该模式考虑了代谢个性、文化背景和数字健康整合。我们的讨论强调了实践和研究重点的关键转变,为临床医生和政策制定者提供了一个及时的框架,以引导糖尿病管理的发展前景。同行评议的文章、临床指南和系统评论均来自PubMed、Scopus和谷歌Scholar等数据库。该分析侧重于评估碳水化合物计数、个性化营养及其各自对血糖控制和患者预后的影响的研究。主要议题包括营养基因组学、代谢组学的进展,以及精准医学在饮食干预中的整合。综合研究结果,突出当前的挑战,新趋势,和潜在的解决方案,在实施个性化的营养策略,糖尿病护理。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Evolving paradigms in nutrition therapy for Diabetes: From carbohydrate counting to precision diets
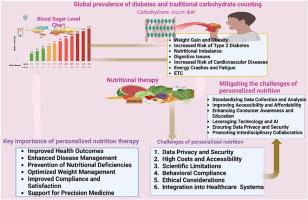
The global prevalence of diabetes is on the rise, necessitating advanced strategies for effective management. Nutrition therapy plays a critical role in managing diabetes, contributing to glycemic control, weight regulation, and complication prevention. Historically centered around carbohydrate counting and standardized meal plans, nutrition strategies have evolved toward more flexible, patient-centered approaches. Emerging evidence underscores the importance of individualized dietary interventions tailored to patients’ cultural preferences, metabolic profiles, and comorbid conditions. Approaches such as the Mediterranean diet, Dietary Approaches to Stop Hypertension (DASH), and plant-based diets have demonstrated significant benefits in both type 1 and type 2 diabetes. The integration of digital tools, behavioral science, and emerging insights from nutrigenomics and the gut microbiome further supports a paradigm shift toward precision nutrition. In this commentary, we highlight the evolution of nutrition therapy in diabetes care, emphasizing the transition from generic recommendations to personalized dietary strategies aimed at improving long-term outcomes. It emphasizes the potential of precision nutrition to optimize glycemic control, mitigate complications, and improve patient adherence. We argue that the future of diabetes care depends on a personalized nutrition model that accounts for metabolic individuality, cultural context, and digital health integration. Our discussion highlights a critical transition in practice and research priorities, offering a timely framework for clinicians and policymakers navigating the evolving landscape of diabetes management. Peer-reviewed articles, clinical guidelines, and systematic reviews were sourced from databases such as PubMed, Scopus, and Google Scholar. The analysis focused on studies evaluating carbohydrate counting, personalized nutrition, and their respective impacts on glycemic control and patient outcomes. Key topics included advancements in nutrigenomics, metabolomics, and the integration of precision medicine in dietary interventions. The findings were synthesized to highlight current challenges, emerging trends, and potential solutions in implementing personalized nutrition strategies for diabetes care.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Obesity Medicine
Medicine-Public Health, Environmental and Occupational Health
CiteScore
5.50
自引率
0.00%
发文量
74
审稿时长
40 days
期刊介绍:
The official journal of the Shanghai Diabetes Institute Obesity is a disease of increasing global prevalence with serious effects on both the individual and society. Obesity Medicine focusses on health and disease, relating to the very broad spectrum of research in and impacting on humans. It is an interdisciplinary journal that addresses mechanisms of disease, epidemiology and co-morbidities. Obesity Medicine encompasses medical, societal, socioeconomic as well as preventive aspects of obesity and is aimed at researchers, practitioners and educators alike.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


