Kosuke Takano, Sayaka Kobayashi, Hidehiro Oshibuchi, Junko Tsutsui, Satoko Ito, Rumiko Kamba, Rie Akaho, Katsuji Nishimura
下载PDF
{"title":"斯坦福移植综合社会心理评估与活体肾移植后1年药物不依从的关系。","authors":"Kosuke Takano, Sayaka Kobayashi, Hidehiro Oshibuchi, Junko Tsutsui, Satoko Ito, Rumiko Kamba, Rie Akaho, Katsuji Nishimura","doi":"10.1002/pcn5.70128","DOIUrl":null,"url":null,"abstract":"<p><strong>Aim: </strong>This study investigated the association between the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT) and medication nonadherence (MNA) in living kidney transplantation (LKT) recipients.</p><p><strong>Methods: </strong>This single-center prospective cohort study included 132 LKT recipients at Tokyo Women's Medical University Hospital between July 2020 and July 2021. Pretransplant psychosocial evaluations used the Japanese version of the SIPAT (SIPAT-J), and MNA was assessed 1 year posttransplant using the Basel Assessment of Adherence to Immunosuppressive Medication Scale<sup>©</sup> (BAASIS<sup>©</sup>). Participants completing both SIPAT-J and BAASIS<sup>©</sup> evaluations (<i>n</i> = 111) were analyzed. Multivariable logistic regression analysis was conducted to examine the relationship between SIPAT scores and MNA, adjusting for age, sex, and employment status.</p><p><strong>Results: </strong>Participants had a median age of 52 years; 63.1% were male. MNA was observed in 39.6% of recipients, primarily due to timing deviations (34.2%) and missed doses (11.7%). Higher SIPAT D (Lifestyle and Effect of Substance Use) scores were significantly associated with MNA (odds ratio = 1.304, 95% confidence interval = 1.006-1.692, P = 0.045). Other SIPAT subscales and total scores were not significantly associated with MNA.</p><p><strong>Conclusion: </strong>To our knowledge, this is the first study to investigate the association between SIPAT and MNA in LKT recipients. MNA remains prevalent 1 year post-LKT, with lifestyle and substance use factors (SIPAT D) showing a significant association. These results underscore the importance of conducting comprehensive psychosocial evaluations, including assessments of lifestyle and substance use, prior to transplantation. Such evaluations may facilitate the identification of at-risk individuals and enable the implementation of targeted interventions to improve medication adherence and posttransplant outcomes.</p>","PeriodicalId":74405,"journal":{"name":"PCN reports : psychiatry and clinical neurosciences","volume":"4 2","pages":"e70128"},"PeriodicalIF":0.9000,"publicationDate":"2025-06-09","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12148955/pdf/","citationCount":"0","resultStr":"{\"title\":\"Association between the Stanford Integrated Psychosocial Assessment for Transplant and 1-year medication nonadherence after living kidney transplantation.\",\"authors\":\"Kosuke Takano, Sayaka Kobayashi, Hidehiro Oshibuchi, Junko Tsutsui, Satoko Ito, Rumiko Kamba, Rie Akaho, Katsuji Nishimura\",\"doi\":\"10.1002/pcn5.70128\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p><strong>Aim: </strong>This study investigated the association between the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT) and medication nonadherence (MNA) in living kidney transplantation (LKT) recipients.</p><p><strong>Methods: </strong>This single-center prospective cohort study included 132 LKT recipients at Tokyo Women's Medical University Hospital between July 2020 and July 2021. Pretransplant psychosocial evaluations used the Japanese version of the SIPAT (SIPAT-J), and MNA was assessed 1 year posttransplant using the Basel Assessment of Adherence to Immunosuppressive Medication Scale<sup>©</sup> (BAASIS<sup>©</sup>). Participants completing both SIPAT-J and BAASIS<sup>©</sup> evaluations (<i>n</i> = 111) were analyzed. Multivariable logistic regression analysis was conducted to examine the relationship between SIPAT scores and MNA, adjusting for age, sex, and employment status.</p><p><strong>Results: </strong>Participants had a median age of 52 years; 63.1% were male. MNA was observed in 39.6% of recipients, primarily due to timing deviations (34.2%) and missed doses (11.7%). Higher SIPAT D (Lifestyle and Effect of Substance Use) scores were significantly associated with MNA (odds ratio = 1.304, 95% confidence interval = 1.006-1.692, P = 0.045). Other SIPAT subscales and total scores were not significantly associated with MNA.</p><p><strong>Conclusion: </strong>To our knowledge, this is the first study to investigate the association between SIPAT and MNA in LKT recipients. MNA remains prevalent 1 year post-LKT, with lifestyle and substance use factors (SIPAT D) showing a significant association. These results underscore the importance of conducting comprehensive psychosocial evaluations, including assessments of lifestyle and substance use, prior to transplantation. Such evaluations may facilitate the identification of at-risk individuals and enable the implementation of targeted interventions to improve medication adherence and posttransplant outcomes.</p>\",\"PeriodicalId\":74405,\"journal\":{\"name\":\"PCN reports : psychiatry and clinical neurosciences\",\"volume\":\"4 2\",\"pages\":\"e70128\"},\"PeriodicalIF\":0.9000,\"publicationDate\":\"2025-06-09\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12148955/pdf/\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"PCN reports : psychiatry and clinical neurosciences\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://doi.org/10.1002/pcn5.70128\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"2025/6/1 0:00:00\",\"PubModel\":\"eCollection\",\"JCR\":\"\",\"JCRName\":\"\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"PCN reports : psychiatry and clinical neurosciences","FirstCategoryId":"1085","ListUrlMain":"https://doi.org/10.1002/pcn5.70128","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"2025/6/1 0:00:00","PubModel":"eCollection","JCR":"","JCRName":"","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Association between the Stanford Integrated Psychosocial Assessment for Transplant and 1-year medication nonadherence after living kidney transplantation.
Aim: This study investigated the association between the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT) and medication nonadherence (MNA) in living kidney transplantation (LKT) recipients.
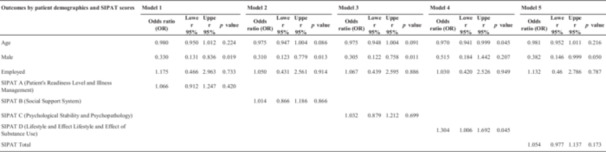
Methods: This single-center prospective cohort study included 132 LKT recipients at Tokyo Women's Medical University Hospital between July 2020 and July 2021. Pretransplant psychosocial evaluations used the Japanese version of the SIPAT (SIPAT-J), and MNA was assessed 1 year posttransplant using the Basel Assessment of Adherence to Immunosuppressive Medication Scale© (BAASIS© ). Participants completing both SIPAT-J and BAASIS© evaluations (n = 111) were analyzed. Multivariable logistic regression analysis was conducted to examine the relationship between SIPAT scores and MNA, adjusting for age, sex, and employment status.
Results: Participants had a median age of 52 years; 63.1% were male. MNA was observed in 39.6% of recipients, primarily due to timing deviations (34.2%) and missed doses (11.7%). Higher SIPAT D (Lifestyle and Effect of Substance Use) scores were significantly associated with MNA (odds ratio = 1.304, 95% confidence interval = 1.006-1.692, P = 0.045). Other SIPAT subscales and total scores were not significantly associated with MNA.
Conclusion: To our knowledge, this is the first study to investigate the association between SIPAT and MNA in LKT recipients. MNA remains prevalent 1 year post-LKT, with lifestyle and substance use factors (SIPAT D) showing a significant association. These results underscore the importance of conducting comprehensive psychosocial evaluations, including assessments of lifestyle and substance use, prior to transplantation. Such evaluations may facilitate the identification of at-risk individuals and enable the implementation of targeted interventions to improve medication adherence and posttransplant outcomes.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


