2005-2023年北爱尔兰儿童通道病:一项主要通过级联筛查确定的国家队列研究
IF 0.8
Q4 PEDIATRICS
引用次数: 0
摘要
背景:遗传性心脏通道病变是由基因变异引起的多种疾病,易使携带者发生心律失常和心脏性猝死(SCD)。例如先天性长QTc (LQTS)、Brugada综合征(BrS)和儿茶酚胺能多态性室性心动过速(CPVT)。目的:在一家遗传性心脏病诊所(ICCC)服务的北爱尔兰儿科人群中,我们描述了渠道病的全国患病率和发病率、临床结果、不良事件、药物使用、药物依从性和获得的遗传数据。方法使用当地儿科心脏病学数据库进行回顾性分析。结果2005年至2023年在ICCC诊断为通道病的儿童216例(0-18岁);190例诊断为LQTS (KCNQ1 116例,KCNH2 36例,SCN5A 11例,KCNE1 19例,2个基因变异3例,KCNE1复合杂合子1例,基因型阴性4例),BrS 22例,CPVT 4例。大多数病例是通过筛查确诊的(95%)。在此期间,有5例记录在案的SCDs,均为ICCC未知的患者,在分子尸检中被诊断为通道病变(2例CPVT, 2例BrS, 1例LQTS)。1例KCNH2患者接受了植入式心律转复除颤器(ICD)植入。在LQTS队列中,大多数人有一种变异(97%)。在KCNQ1患者中鉴定出22个变体,KCNH2患者中鉴定出14个,SCN5A患者中鉴定出2个,KCNE1患者中鉴定出7个。正如预期的那样,表型异质性在变异之间和变异内部被注意到。药物依从性在70%到90%之间。结论一般来说,北爱尔兰儿童的经道病是通过家庭筛查诊断的,并开始适当的药物治疗,不良事件很少发生。基因图谱与世界范围内报道的大致相似。不幸的是,仍然有一群患者只能通过分子解剖来识别。本文章由计算机程序翻译,如有差异,请以英文原文为准。
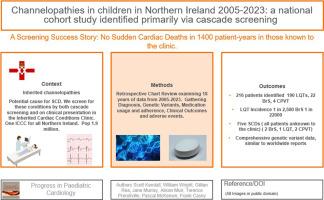
Channelopathies in children in Northern Ireland 2005–2023: A national cohort study identified primarily via cascade screening
Background
The inherited cardiac channelopathies are a diverse range of conditions caused by genetic variants that predispose carriers to arrhythmia and sudden cardiac death (SCD). Examples include Congenital Long QTc (LQTS), Brugada syndrome (BrS), and Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT).
Objective
In the Northern Ireland pediatric population, served by one inherited cardiac conditions clinic (ICCC), we describe the national prevalence and incidence of the channelopathies, clinical outcomes, adverse events, medication usage, medication adherence, and genetic data obtained.
Methods
Retrospective chart review using the local pediatric cardiology database.
Results
216 children (Aged 0–18) were diagnosed with a channelopathy between 2005 and 2023 at the ICCC; 190 were diagnosed with LQTS (116 KCNQ1, 36 KCNH2, 11 SCN5A, 19 KCNE1, 3 patients with variants in two genes, 1 compound heterozygote for KCNE1 and 4 genotype negative), 22 with BrS and 4 with CPVT. Most cases were diagnosed via screening (95 %). There were five documented SCDs during this time, all patients unknown to the ICCC, who were diagnosed with channelopathies on molecular autopsy (2 CPVT, 2 BrS, 1 LQTS). One KCNH2 patient underwent implantable cardioverter defibrillator (ICD) insertion. In the LQTS cohort, the majority had a variant identified (97 %). Twenty-two variants were identified in KCNQ1 patients, fourteen in KCNH2, two in SCN5A, and seven in KCNE1. As would be expected, phenotype heterogeneity was noted between and within variants. Adherence with medication varied between 70 and 90 %.
Conclusions
In general, children with channelopathies in Northern Ireland (NI) are diagnosed via family screening, commenced on appropriate pharmacotherapy, and adverse events are rare. The genetic profile is broadly similar to that reported worldwide. Unfortunately, there remains a cohort of patients who are only identified at molecular autopsy.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

PROGRESS IN PEDIATRIC CARDIOLOGY
PEDIATRICS-
CiteScore
0.90
自引率
11.10%
发文量
69
审稿时长
75 days
期刊介绍:
Progress in Pediatric Cardiology is an international journal of review presenting information and experienced opinion of importance in the understanding and management of cardiovascular diseases in children. Each issue is prepared by one or more Guest Editors and reviews a single subject, allowing for comprehensive presentations of complex, multifaceted or rapidly changing topics of clinical and investigative interest.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


