抗il - 17治疗化脓性汗腺炎的安全性和有效性:随机安慰剂对照试验的系统评价和荟萃分析。
IF 2.8
Q1 DERMATOLOGY
引用次数: 0
摘要
背景与目的:化脓性汗腺炎(HS)是一种难以控制的慢性炎症性皮肤病,需要使用抗tnf α和抗白细胞介素17 (anti- il - 17)等生物药物。我们回顾的目的是评估抗il - 17药物在HS患者中的安全性和有效性。材料和方法:我们根据人群、干预、比较、结果和研究类型(PICOS)方法进行了系统综述和随后的荟萃分析。我们只纳入了随机临床试验安慰剂(S),包括HS bb0 - 18岁(P)的个体,并且已经服用安慰剂(C)或抗il - 17生物药物(I)来衡量安全性和有效性结果(O)。检索是在多个数据库中进行的:PubMed, Scopus和Cochrane中央对照试验登记册。确定了每项研究的偏倚风险、发表偏倚、敏感性分析和证据的确定性。结果:共获取文献320篇,其中符合纳入标准的文献4篇。与安慰剂相比,荟萃分析显示,达到化脓性汗腺炎临床反应(HiSCR) OR的患者比例显著更高,为1.96 [1.79-2.15],DLQI下降幅度更大,MD下降-1.92[-2.68,-1.16],不良反应增加;OR为1.21[1.09,1.34],特别是念珠菌感染;或者,5.61[2.66-11.83]。结论:抗il - 17生物药物治疗中重度HS是有效的。虽然这些药物是安全的,但由于感染(主要是念珠菌病)的风险,应对其进行监测。本文章由计算机程序翻译,如有差异,请以英文原文为准。
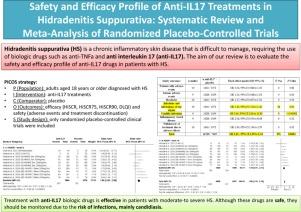
Safety and Efficacy Profile of Anti-IL17 Treatments in Hidradenitis Suppurativa: Systematic Review and Meta-Analysis of Randomized Placebo-Controlled Trials
Background and objective
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that is difficult to manage, requiring the use of biologic drugs such as anti-TNFα and anti-interleukin 17 (anti-IL17). The aim of our review is to evaluate the safety and efficacy profile of anti-IL17 drugs in patients with HS.
Materials and methods
We conducted a systematic review with subsequent meta-analysis following the population, intervention, comparison, outcome and type of study (PICOS) method. We included only randomized clinical trials with placebo (S) that included individuals with HS ≥ 18 years old (P), and who had been on placebo (C) OR, an anti-IL17 biologic drug (I) to measure safety and efficacy outcomes (O). Search was conducted across multiple databases: PubMed, Scopus, and the Cochrane Central Register of Controlled Trials. The risk of bias of each study, publication bias, sensitivity analysis, and certainty of evidence were determined.
Results
A total of 320 bibliographic references were obtained, 4 of which met the inclusion criteria. Compared to placebo, the meta-analysis showed a significantly higher percentage of patients achieving Hidradenitis Suppurativa Clinical Response (HiSCR) OR, of 1.96 [1.79–2.15], a greater decrease in DLQI, MD −1.92 [−2.68,−1.16] and an increase in adverse effects; OR, 1.21 [1.09, 1.34], particularly due to Candida infections; OR, 5.61 [2.66–11.83].
Conclusions
Treatment with anti-IL17 biologic drugs is effective in patients with moderate-to-severe HS. Although these drugs are safe, they should be monitored due to the risk of infections, mainly candidiasis.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Actas dermo-sifiliograficas
DERMATOLOGY-
CiteScore
1.90
自引率
9.40%
发文量
473
审稿时长
56 weeks
期刊介绍:
Actas Dermo-Sifiliográficas, publicación Oficial de la Academia Española de Dermatología y Venereología, es una revista de prestigio consolidado. Creada en 1909, es la revista mensual más antigua editada en España.En 2006 entró en Medline, y hoy resulta imprescindible para estar al día sobre la dermatología española y mundial.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


