脂肪变性肝病亚群具有不同的临床表型
IF 3.2
Q2 GASTROENTEROLOGY & HEPATOLOGY
Journal of Clinical and Experimental Hepatology
Pub Date : 2025-04-30
DOI:10.1016/j.jceh.2025.102587
引用次数: 0
摘要
背景和目的脂肪变性肝病(SLD)描述了由心脏代谢危险因素(CMRF)和/或酒精引起的一系列肝脏疾病。我们的目的是描述累积CMRF和酒精对SLD亚组的影响,并比较临床结果。方法回顾性纳入来自单一中心活检证实的SLD患者。根据共识定义将患者分为三个SLD亚组。考虑竞争风险,分析随访期间肝相关性死亡或肝移植的风险。将CMRF和酒精摄入量的顺序组的结果制成表格。结果纳入726例患者:516例(71%)患有代谢功能障碍相关脂肪变性肝病(MASLD), 85例(12%)MASLD伴酒精摄入量增加(MetALD), 125例(17%)患有ALD。患者的中位随访时间为60.5个月(IQR 29-84.5),期间64例(8.8%)患者死亡,包括23例肝脏相关死亡。竞争风险回归分析显示,与MASLD相比,ALD与肝脏相关死亡的风险更高,sHR为8.47 (95% CI, 2.26-31.8, P = 0.002)。主要不良肝脏结局或肝脏相关死亡的风险随着CMRF的数量和酒精的增加而增加,显示出这些因素对患者结局的协同作用。结论在SLD患者中,ALD患者发生不良肝脏结局的风险最大。相反,在中短期内,与肝脏相关的结果在MASLD中不太常见。这强调有必要将酒精滥用作为不良后果的一个重要风险因素加以识别和治疗。本文章由计算机程序翻译,如有差异,请以英文原文为准。
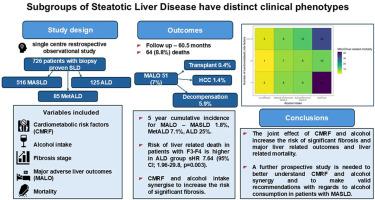
Subgroups of Steatotic Liver Disease Have Distinct Clinical Phenotypes
Background and aims
Steatotic liver disease (SLD) describes a spectrum of liver disease caused by cardiometabolic risk factors (CMRF) and/or alcohol. We aimed to describe the effect of cumulative CMRF and alcohol in subgroups of SLD and compare clinical outcomes.
Methods
Patients from a single centre with biopsy proven SLD were retrospectively included. Patients were classified according to consensus definitions into three subgroups of SLD. The risk of liver-related death or liver transplantation during follow-up was analysed considering competing risks. Outcomes were tabulated for ordinal groups of CMRF and alcohol intake.
Results
726 patients were included: 516 (71%) had metabolic dysfunction-associated steatotic liver disease (MASLD), 85 (12%) MASLD with increased alcohol intake (MetALD), and 125 (17%) had ALD. Patients were followed up for a median of 60.5 months (IQR 29–84.5), during which time 64 (8.8%) patients died, including 23 liver-related deaths. Competing risk regression analysis showed that ALD was associated with higher risk of liver-related death sHR 8.47 (95% CI, 2.26–31.8, P = 0.002) compared to MASLD. The risk of major adverse liver outcomes or liver-related death increased with the number of CMRF and with alcohol, showing a synergistic effect of these factors on patient outcomes.
Conclusions
Amongst patients with SLD, patients with ALD have the greatest risk of adverse liver outcomes. Conversely, liver-related outcomes are less common in MASLD in the short to medium-term. This emphasises the need to identify and treat alcohol misuse as an important risk factor for adverse outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Clinical and Experimental Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.90
自引率
16.70%
发文量
537
审稿时长
64 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


