立体定向体放射治疗晚期肝内胆管癌:来自印度队列的真实世界结果
IF 3.2
Q2 GASTROENTEROLOGY & HEPATOLOGY
Journal of Clinical and Experimental Hepatology
Pub Date : 2025-04-28
DOI:10.1016/j.jceh.2025.102584
引用次数: 0
摘要
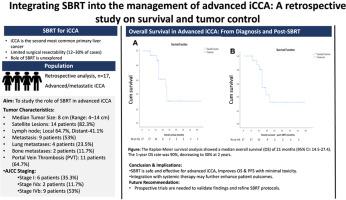
肝性胆管癌(iCCA)是第二常见的原发性肝脏恶性肿瘤,占胃肠道肿瘤的3%。虽然手术切除提供25-40%的五年总生存率(OS),但只有12-30%的病例是可切除的。晚期或转移性iCCA通常需要全身治疗结合局部区域治疗,如立体定向全身放射治疗(SBRT)。尽管SBRT有改善局部控制(LC)和OS的潜力,但其作用在很大程度上仍未被探索,特别是与全身治疗的整合。本研究评估了SBRT在晚期/转移性iCCA中提高LC和OS的作用,重点是SBRT与全身治疗的结合。方法回顾性分析2019年至2024年间治疗的17例晚期/转移性iCCA患者。从电子病历中获得基线特征、治疗方案和结果。SBRT的剂量范围为30至50 Gy,分5-10个分数施用。每三个月进行一次随访评估,以评估LC、疾病进展和生存。统计分析,包括Kaplan-Meier生存估计,使用SPSS 23.0进行,p值为<;0.05认为显著。结果中位随访时间为14个月。诊断后的中位生存期为21个月(95% CI: 14.5-27.4), 1年和2年生存期分别为90%和30%。中位无进展生存期(PFS)为10个月(95% CI: 8.1-11.8), 1年和2年PFS率分别为35%和15%。1年和2年的LC率分别为92%和70%。性别显著影响OS,有利于女性患者。治疗耐受性良好,无sbrt相关胆管炎或肝功能衰竭。结论sbrt似乎是一种安全且潜在有益的晚期/转移性iCCA治疗方法,在毒性最小的情况下可能改善OS和PFS。这项研究强调了将SBRT与全身治疗相结合的潜力,特别是在有大量肿瘤负担的患者中。需要进一步的前瞻性试验来验证这些发现并完善晚期iCCA的SBRT方案。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Stereotactic Body Radiation Therapy in Advanced Intrahepatic Cholangiocarcinoma: Real-world Outcomes from an Indian Cohort
Background
Intrahepatic cholangiocarcinoma (iCCA), the second most common primary liver malignancy, accounts for 3% of gastrointestinal cancers. While surgical resection offers a five-year overall survival (OS) of 25–40%, only 12–30% of cases are resectable. Advanced or metastatic iCCA often necessitates systemic therapy combined with loco-regional treatments such as stereotactic body radiation therapy (SBRT). Despite its potential to improve local control (LC) and OS, the role of SBRT remains largely unexplored, particularly its integration with systemic therapy. This study evaluates the role of SBRT, with a focus on its combination with systemic therapy, in enhancing LC and OS in advanced/metastatic iCCA.
Methodology
This retrospective analysis included 17 patients with advanced/metastatic iCCA treated between 2019 and 2024. Baseline characteristics, treatment regimens, and outcomes were obtained from electronic medical records. SBRT was administered in doses ranging from 30 to 50 Gy over 5–10 fractions. Follow-up assessments were conducted every three months to evaluate LC, disease progression, and survival. Statistical analyses, including Kaplan–Meier survival estimates, were performed using SPSS 23.0, with a P-value of <0.05 considered significant.
Results
The median follow-up was 14 months. The median OS was 21 months (95% CI: 14.5–27.4) from diagnosis, with one- and two-year OS rates of 90% and 30%, respectively. The median progression-free survival (PFS) was 10 months (95% CI: 8.1–11.8), with one- and two-year PFS rates of 35% and 15%, respectively. LC rates at one and two years were 92% and 70%, respectively. Gender significantly impacted OS, favoring female patients. Treatment was well tolerated, with no SBRT-related cholangitis or liver failure.
Conclusion
SBRT appears to be a safe and potentially beneficial approach for advanced/metastatic iCCA, suggesting potential improvements in OS and PFS with minimal toxicity. This study highlights the potential of integrating SBRT with systemic therapies, particularly in patients with substantial tumor burden. Further prospective trials are necessary to validate these findings and refine SBRT protocols for advanced iCCA.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Clinical and Experimental Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.90
自引率
16.70%
发文量
537
审稿时长
64 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


