肠道菌群与化脓性关节炎之间的因果关系:一项双样本孟德尔随机研究。
摘要
介绍。越来越多的证据表明,肠道微生物群与发生化脓性关节炎(PA)的风险之间存在显著关联。然而,它们之间的因果关系还有待阐明。肠道菌群与患paa的风险有因果关系。采用孟德尔随机化(MR)方法评估肠道菌群对pa易感性的潜在因果影响。使用MiBioGen联盟进行的最大的全基因组关联研究荟萃分析(n=13,266)的肠道微生物群汇总统计数据进行了两样本MR研究。PA的汇总统计数据来自FinnGen联盟提供的R11发布数据(2441例,对照287796例)。采用反方差加权(IVW)模型、加权中位数估计模型、基于加权模型的方法和MR-Egger回归(MER)模型检验肠道菌群与PA的因果关系。为了评估识别工具变量(IVs)的异质性和多效性效应,我们使用了几种分析方法,包括留一敏感性分析、MR多效性残差和异常值检验和科克伦Q检验。利用IVW方法,我们鉴定出6个与PA呈负相关的细菌性状:真杆菌群[OR: 0.6057;95%置信区间(CI): 0.4525 ~ 0.8107;P=0.0007],巴氏菌(OR: 0.7456;95% CI: 0.5760 ~ 0.9651;P=0.0258), Coprococcus2 (OR: 0.7257;95% CI: 0.5352 - 0.9840;P=0.0391),瘤胃球菌科UCG005 (OR: 0.7562;95% CI: 0.5920 ~ 0.9660;P=0.0252), E. oxidreducens组(OR: 0.7311;95% CI: 0.5547 ~ 0.9637;P=0.0262)和毛缕科FCS020组(OR: 0.7825;95% CI: 0.6135 ~ 0.9981;分别P = 0.0482)。相反,4种细菌性状与PA呈显著正相关:Adlercreutzia (OR 1.3210, 95% CI 1.0181 ~ 1.7141, P=0.0362)、Holdemania (OR 1.2239, 95% CI 1.0013 ~ 1.4960, P=0.0485)、厌氧菌(OR 1.3614, 95% CI 1.0189 ~ 1.8191, P=0.0369)和Butyricimonas (OR 1.2627, 95% CI 1.0016 ~ 1.5921, P=0.0484)。各组间未发现明显的异质性或水平多效性。我们的研究表明,各种肠道微生物群与PA风险之间存在潜在的因果关系。肠道菌群影响PA发病的机制有待进一步研究。
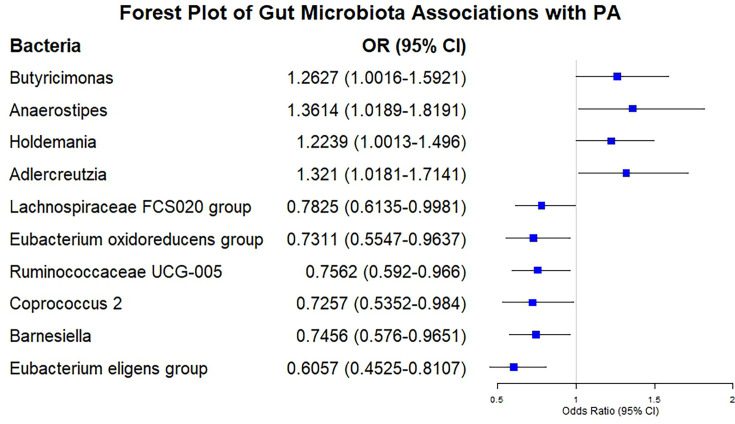
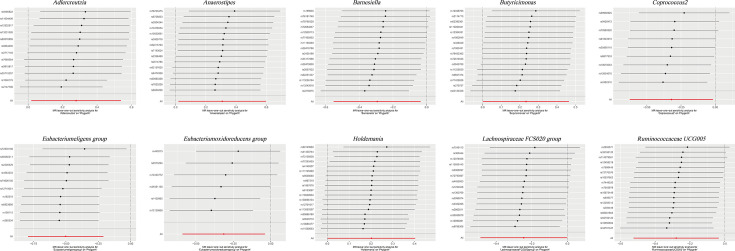
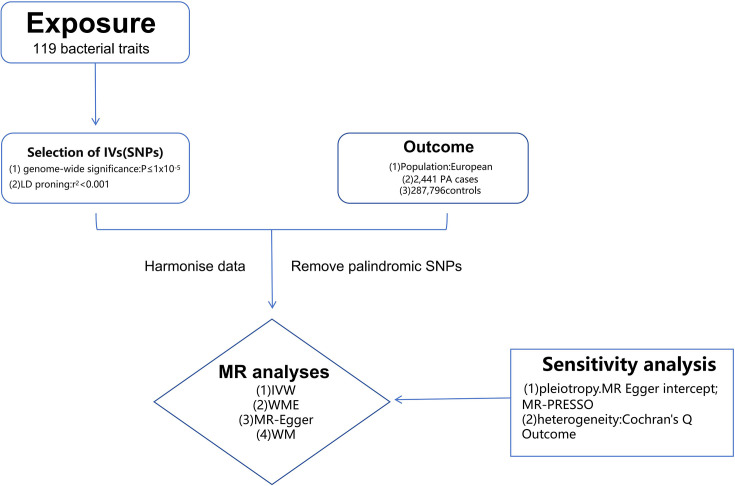
Introduction. Accumulating evidence indicates a significant association between gut microbiota and the risk of developing pyogenic arthritis (PA). However, their causal relationship has yet to be elucidated.Hypothesis. The gut microbiota is causally associated with the risk of PA.Aim. The Mendelian randomization (MR) methodology was employed to assess the potential causal effects of gut microbiota on the susceptibility to PA.Methodology. A two-sample MR study was performed using the summary statistics of gut microbiota from the largest available genome-wide association study meta-analysis (n=13,266) conducted by the MiBioGen consortium. The summary statistics of PA were obtained from the R11 release data provided by the FinnGen consortium (2,441 cases and 2,87,796 controls). Inverse-variance weighted (IVW) model, weighted median estimator model, weighted model-based method and MR-Egger regression (MER) model were used to examine the causal association between gut microbiota and PA. To assess the heterogeneity and pleiotropic effects of the identified instrumental variables (IVs), we utilized several analytical methods, including the leave-one-out sensitivity analysis, the MR Pleiotropy Residual Sum and Outlier test and Cochran's Q test.Results. Utilizing the IVW method, we identified six bacterial traits that were negatively correlated with PA: Eubacterium eligens group [OR: 0.6057; 95 % confidence interval (CI): 0.4525 to 0.8107; P=0.0007], Barnesiella (OR: 0.7456; 95 % CI: 0.5760 to 0.9651; P=0.0258), Coprococcus2 (OR: 0.7257; 95 % CI: 0.5352 to 0.9840; P=0.0391), Ruminococcaceae UCG005 (OR: 0.7562; 95 % CI: 0.5920 to 0.9660; P=0.0252), E. oxidoreducens group (OR: 0.7311; 95 % CI: 0.5547 to 0.9637; P=0.0262) and Lachnospiraceae FCS020 group (OR: 0.7825; 95 % CI: 0.6135 to 0.9981; P=0.0482), respectively. On the contrary, four bacterial traits were positively correlated with PA: Adlercreutzia (OR 1.3210, 95 % CI 1.0181-1.7141, P=0.0362), Holdemania (OR 1.2239, 95 % CI 1.0013-1.4960, P=0.0485), Anaerostipes (OR 1.3614, 95 % CI 1.0189-1.8191, P=0.0369) and Butyricimonas (OR 1.2627, 95 % CI 1.0016-1.5921, P=0.0484), respectively. No significant heterogeneity among IVs or evidence of horizontal pleiotropy was detected.Conclusion. Our research demonstrates a potential causal link between various gut microbiota and the risk of PA. Further research is imperative to elucidate the mechanisms by which gut microbiota influence the pathogenesis of PA.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


