氰基丙烯酸酯关闭下肢浅静脉患者超敏反应的回顾性研究。
IF 2.8
2区 医学
Q2 PERIPHERAL VASCULAR DISEASE
Journal of vascular surgery. Venous and lymphatic disorders
Pub Date : 2025-04-09
DOI:10.1016/j.jvsv.2025.102246
引用次数: 0
摘要
目的:慢性静脉功能不全影响超过2500万美国成年人,他们最初表现为静脉曲张。尽管存在以热为基础的微创静脉内手术,但最近出现了用于静脉消融的非热静脉内方法,如使用VenaSeal关闭系统的氰基丙烯酸酯关闭(CAC),可降低热损伤的风险。本研究旨在确定CAC后超敏反应(HSRs)的发生率、发作、持续时间和严重程度,并确定发生HSRs的危险因素。方法:本研究在马萨诸塞州布里格姆总医院进行,纳入2018年至2022年期间治疗的122例患者,共193例静脉。患者年龄在18岁及以上,有症状且下肢浅静脉功能不全,包括大隐静脉、小隐静脉和前副隐静脉。收集了患者人口统计学、临床病史、手术细节和术后双工超声结果的数据。结果:在该队列中,HSRs的发生率为21.2%。症状平均发生在手术后7.6天(标准差为7.4天),大多数患者出现轻度(76%)或中度(24%)症状,无需干预、非甾体抗炎药或类固醇治疗即可缓解。年龄越小(P = .0372)、性别越低(P = .0025)、有过敏史(P = .0049)的人群发生HSRs的风险越高。较长的静脉(P = 0.0205)和较大的隐静脉(P = 0.088)与hsr的相关性较强。CAC术后总体闭合率为99.5%,有HSRs和没有HSRs的患者之间无显著差异。结论:HSRs是CAC手术的潜在不良并发症,大多数病例是自限性的,影响个体,年轻,女性,有过敏史。这些发现表明,在考虑采用CAC手术治疗慢性静脉功能不全时,需要仔细选择患者并进行咨询。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Retrospective study of hypersensitivity reactions in patients undergoing cyanoacrylate closure of lower extremity superficial veins
Objective
Chronic venous insufficiency affects more than 25 million adults in the United States, who initially presents with varicose veins. Although thermal-based, minimally invasive endovenous procedures exist, there has been a recent advent of non-thermal endovenous methods for vein ablation such as cyanoacrylate closure (CAC) with the VenaSeal Closure System, which decreases the risk of thermal injury. This study aimed to determine the incidence, onset, duration, and severity of hypersensitivity reactions (HSRs) following CAC, as well as identify risk factors for the development of HSRs.
Methods
This study was conducted at the Massachusetts General Brigham health care system and included 122 patients with 193 veins treated between 2018 and 2022. Patients aged 18 years and older with symptomatic, incompetent superficial lower extremity veins, including the great saphenous vein, small saphenous vein, and anterior accessory saphenous vein, were included. Data on patient demographics, clinical history, procedure details, and post-procedural duplex ultrasound results were collected.
Results
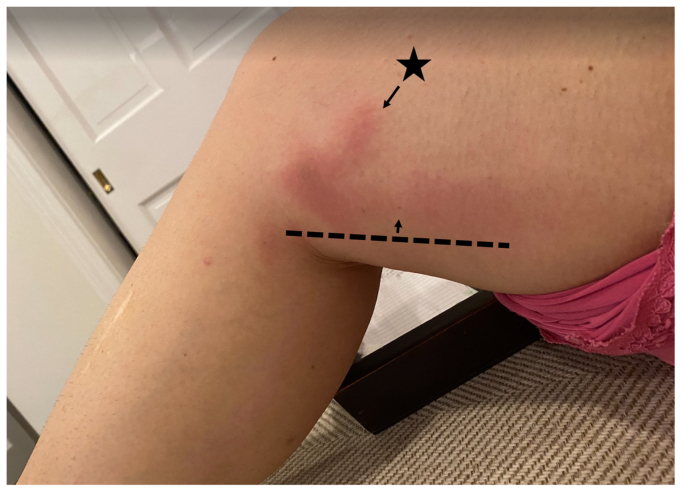
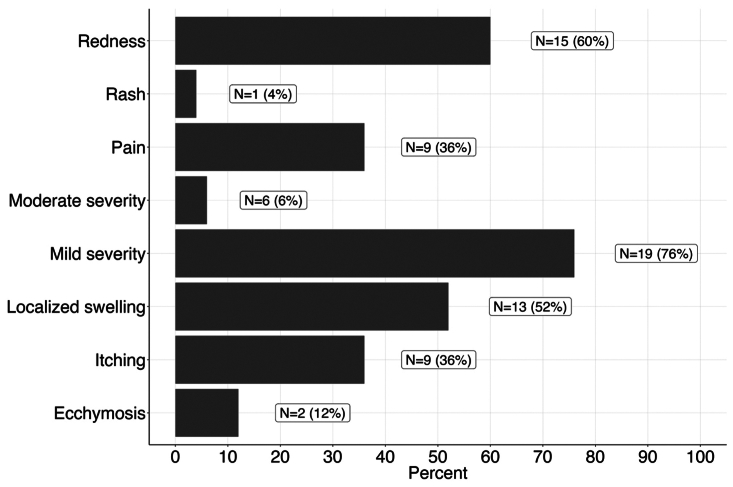
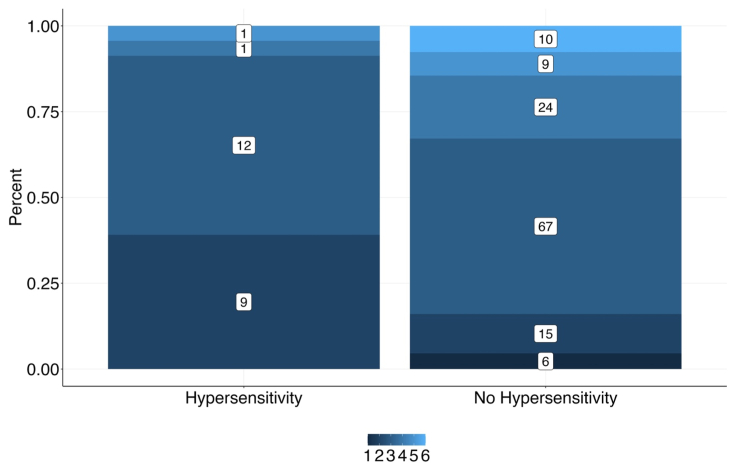
In this cohort, the incidence of HSRs was 21.2%. Symptom onset occurred on average 7.6 days post-procedure (standard deviation, 7.4 days) with most patients experiencing mild (76%) or moderate (24%) symptoms that resolved without intervention, with non-steroidal anti-inflammatory drugs, or with steroid treatment. There was a significantly higher risk of HSRs with younger age (P = .0372), female sex (P = .0025), and history of allergies (P = .0049). Longer veins (P = .0205) and greater saphenous veins (P = .0388) had stronger associations with HSRs. The overall postoperative closure rate after CAC procedure was 99.5%, without a significant difference between patients with and without HSRs.
Conclusions
HSRs are a potential adverse complication of the CAC procedure, with most cases being self-limited and affecting individuals who are younger, are female, and have a history of allergies. These findings suggest the need for careful patient selection and counseling during consideration of the CAC procedure for the treatment of chronic venous insufficiency.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of vascular surgery. Venous and lymphatic disorders
SURGERYPERIPHERAL VASCULAR DISEASE&n-PERIPHERAL VASCULAR DISEASE
CiteScore
6.30
自引率
18.80%
发文量
328
审稿时长
71 days
期刊介绍:
Journal of Vascular Surgery: Venous and Lymphatic Disorders is one of a series of specialist journals launched by the Journal of Vascular Surgery. It aims to be the premier international Journal of medical, endovascular and surgical management of venous and lymphatic disorders. It publishes high quality clinical, research, case reports, techniques, and practice manuscripts related to all aspects of venous and lymphatic disorders, including malformations and wound care, with an emphasis on the practicing clinician. The journal seeks to provide novel and timely information to vascular surgeons, interventionalists, phlebologists, wound care specialists, and allied health professionals who treat patients presenting with vascular and lymphatic disorders. As the official publication of The Society for Vascular Surgery and the American Venous Forum, the Journal will publish, after peer review, selected papers presented at the annual meeting of these organizations and affiliated vascular societies, as well as original articles from members and non-members.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


