用PCSK9抑制剂开始降脂治疗后视网膜微血管功能的改善-一项观察性研究。
IF 4.6
3区 医学
Q2 PHARMACOLOGY & PHARMACY
引用次数: 0
摘要
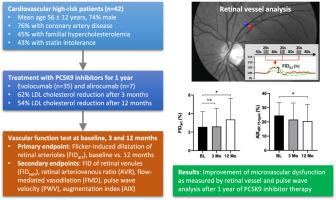
背景:高胆固醇血症与内皮功能障碍有关。虽然有充分的证据表明他汀类药物对内皮的有益作用,但对一类新的蛋白转化酶枯草杆菌素/ keexin型9 (PCSK9)抑制剂知之甚少。目的:本研究的目的是研究PCSK9抑制剂对微、大血管内皮功能和动脉硬度指标的影响。方法:在这项前瞻性观察研究中,测量心血管高危患者的视网膜微血管功能、肱动脉血流介导的扩张(FMD)和动脉刚度(脉搏波速度[PWV];PCSK9抑制剂治疗3个月和12个月后的增强指数[AI])。主要终点是12个月后与基线相比,闪烁诱导的视网膜小动脉扩张(FIDart)的变化。结果:最终研究队列包括42例患者(平均年龄56±12岁;男性74%;76%是冠状动脉疾病)。12个月后低密度脂蛋白(LDL)胆固醇由3.8±1.2降至1.8±0.9 mmol/L。PCSK9抑制剂治疗后,视网膜微血管功能(FIDart基线值为2.6%±1.6%,12个月后为3.4%±2.3%,p = 0.01)和AI(基线值为24%±9%,12个月后为21%±12%,p = 0.03)显著改善。FMD、PWV和其他视网膜血管测量没有明显变化。结论:在心血管高危患者中,PCSK9抑制与视网膜闪烁诱导的扩张和AI的改善有关,从而将LDL降低与微血管功能的改善联系起来。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Improvement of retinal microvascular function after initiation of lipid-lowering therapy with PCSK9 inhibitors - An observational study
BACKGROUND
Hypercholesterolemia is associated with endothelial dysfunction. While good evidence exists for the beneficial endothelial effects of statins, less is known on the new class of proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors.
OBJECTIVE
The goal of this study was to study the effects of PCSK9 inhibitors on markers of micro- and macrovascular endothelial function and arterial stiffness.
METHODS
In this prospective observational study, cardiovascular high-risk patients were measured for retinal microvascular function, brachial artery flow-mediated dilatation (FMD), and arterial stiffness (pulse wave velocity [PWV]; augmentation index [AI]) at baseline and after 3 and 12 months of PCSK9 inhibitor therapy. The primary endpoint was the change in flicker-induced dilatation of retinal arterioles (FIDart) after 12 months compared to baseline.
RESULTS
The final study cohort included 42 patients (mean age 56 ± 12 years; 74% male; 76% coronary artery disease). Low-density lipoprotein (LDL) cholesterol was reduced from 3.8 ± 1.2 to 1.8 ± 0.9 mmol/L after 12 months. Retinal microvascular function (FIDart 2.6% ± 1.6% at baseline vs 3.4% ± 2.3% after 12 months, p = .01) and AI (24% ± 9% at baseline vs 21% ± 12% after 12 months, p = .03) improved significantly on PCSK9 inhibitor therapy. No significant changes were observed for FMD, PWV, and other retinal vascular measurements.
CONCLUSION
In cardiovascular high-risk patients, PCSK9 inhibition is associated with an improvement of retinal flicker-induced dilatation and AI, thereby linking LDL lowering with improvement of microvascular function.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
7.00
自引率
6.80%
发文量
209
审稿时长
49 days
期刊介绍:
Because the scope of clinical lipidology is broad, the topics addressed by the Journal are equally diverse. Typical articles explore lipidology as it is practiced in the treatment setting, recent developments in pharmacological research, reports of treatment and trials, case studies, the impact of lifestyle modification, and similar academic material of interest to the practitioner.
Sections of Journal of clinical lipidology will address pioneering studies and the clinicians who conduct them, case studies, ethical standards and conduct, professional guidance such as ATP and NCEP, editorial commentary, letters from readers, National Lipid Association (NLA) news and upcoming event information, as well as abstracts from the NLA annual scientific sessions and the scientific forums held by its chapters, when appropriate.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


