左束支区起搏优化心脏再同步化治疗(LOT-CRT)与传统CRT的超声心动图反应。
IF 5.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
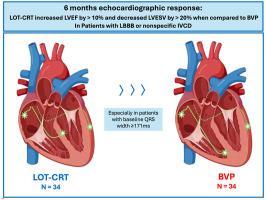
背景:传统的心脏再同步化治疗(CRT)与双心室起搏(BVP)可能对非特异性脑室传导延迟(NIVCD)患者效果较差。左束支区起搏(LBBAP)联合左室冠状静脉导联起搏(LOT-CRT)可能对这些患者更有效。目的:我们评估了左束支阻滞(LBBB)或NIVCD患者的LOT-CRT超声心动图反应,并与倾向匹配的BVP队列进行了比较。方法:选择常规CRT指征患者,优先选择NIVCD患者。超声心动图参数,包括左室射血分数(LVEF)的绝对百分比变化和左室收缩末期容积(LVESV)的相对百分比变化,在植入和6个月的随访中进行评估。BVP队列来自一项独立研究,采用1:1倾向匹配选择。LOT-CRT患者被细分为“成功的LOT-CRT”(LBBAP;电极心电图V1中r′的存在)和“DOT-CRT”(功能性深间隔捕获)。结果:LOT-CRT患者(N=34;年龄64岁,女性38%,NIVCD 47%, LBBB 53%, ICM 21%, QRSd 175 ms, LVEF 27.6%)患者的LVEF改善显著(16.1% vs 6.1%);结论:与BVP相比,NIVCD和LBBB患者的LVEF和LVESV改善更佳,并增强了CRT反应。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Echocardiographic response from left bundle branch area pacing optimized cardiac resynchronization therapy (LOT-CRT) vs traditional CRT
Background
Traditional cardiac resynchronization therapy (CRT) with biventricular pacing (BVP) may be less effective in patients with nonspecific intraventricular conduction delay (NIVCD). Left bundle branch area pacing (LBBAP) combined with left ventricular (LV) coronary venous lead pacing (LOT-CRT) may be more effective in these patients.
Objective
We assessed the echocardiographic response of LOT-CRT in patients with left bundle branch block (LBBB) or NIVCD and compared it with a propensity-matched BVP cohort.
Methods
Patients with conventional CRT indications and preferentially NIVCD were recruited. Echocardiographic parameters, including absolute percentage change in LV ejection fraction (LVEF) and relative percentage change in LV end-systolic volume (LVESV), were evaluated at implantation and 6-month follow-up. The BVP cohort was from an independent study, selected using 1:1 propensity-matching. LOT-CRT patients were subclassified into “successful LOT-CRT” (LBBAP; presence of r’ in electrode electrocardiography [ECG] V1) and “deep septal optimized therapy” (DOT-CRT) (functional deep septal capture).
Results
LOT-CRT patients (N = 34; age 64 years, women 38%, NIVCD 47%, LBBB 53%, implantable cardiac monitor 21%, QRSd 175 ms, and LVEF 27.6%) had significantly greater LVEF improvement (16.1% vs 6.1%; P <.01) and LVESV reduction (−43.5% vs −20.9%; P <.01) compared with BVP patients. After adjusting for baseline characteristics, LOT-CRT patients still had significantly greater LVEF improvement (7.5%; P <.01) and LVESV reduction (18.4%; P <.01) than BVP patients. The response was consistent across LBBB and NIVCD subgroups. LOT-CRT patients with QRS ≥ 171 ms showed greater benefit (P = .04; both LVEF and LVESV). No significant differences were observed between successful LOT-CRT and DOT-CRT.
Conclusion
LOT-CRT resulted in superior LVEF and LVESV improvements compared with BVP in NIVCD and LBBB patients and enhanced CRT response.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Heart rhythm
医学-心血管系统
CiteScore
10.50
自引率
5.50%
发文量
1465
审稿时长
24 days
期刊介绍:
HeartRhythm, the official Journal of the Heart Rhythm Society and the Cardiac Electrophysiology Society, is a unique journal for fundamental discovery and clinical applicability.
HeartRhythm integrates the entire cardiac electrophysiology (EP) community from basic and clinical academic researchers, private practitioners, engineers, allied professionals, industry, and trainees, all of whom are vital and interdependent members of our EP community.
The Heart Rhythm Society is the international leader in science, education, and advocacy for cardiac arrhythmia professionals and patients, and the primary information resource on heart rhythm disorders. Its mission is to improve the care of patients by promoting research, education, and optimal health care policies and standards.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


