经颈静脉肝内门静脉系统分流治疗肝硬化门静脉血栓形成的可行性、安全性和有效性
IF 3.2
Q2 GASTROENTEROLOGY & HEPATOLOGY
Journal of Clinical and Experimental Hepatology
Pub Date : 2025-04-12
DOI:10.1016/j.jceh.2025.102580
引用次数: 0
摘要
背景,目的抗凝治疗被认为是肝硬化门静脉血栓形成(PVT)的标准治疗;然而,尽管抗凝治疗,仍有相当数量的患者不能安全治疗或表现出血栓进展。我们评估了经颈静脉肝内门静脉系统分流术(TIPS)在肝硬化PVT治疗中的作用。方法回顾性研究所有在三级保健中心接受TIPS治疗的肝硬化非肿瘤性PVT患者。排除PVT患者和TIPS的其他适应症。分析了该方法的可行性、安全性和有效性。TIPS的结果与一项针对难治性腹水的TIPS患者的当代队列比较。结果研究期间共243例患者行TIPS治疗,其中30例仅行门静脉再通。40%的患者存在门脉海绵瘤,53%的患者有Yerdel 3或4型pvt。TIPS的主要适应症是禁忌症(53%)或抗凝治疗缺乏反应(30%)。在17%的病例中,当PVT阻止门静脉吻合时,提示TIPS可以促进肝移植(LT)。TIPS的成功率为96.6%。TIPS后的主要并发症(2例)和分流相关事件与对照组相似。17%的患者表现出TIPS功能障碍(全部成功治疗),这一比例与难治性腹水患者相似。tips术后门静脉压力梯度越高,功能障碍风险越大。所有患者门静脉主干均保持通畅,其中8例患者接受了平稳的lt治疗。结论tips可以安全地用于肝硬化和PVT患者,如果药物治疗失败或有禁忌症,则有再通的指征。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Feasibility, Safety and Efficacy of Transjugular Intrahepatic Portosystemic Shunt for the Management of Portal Vein Thrombosis in Cirrhosis
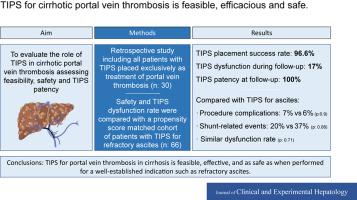
Background & aims
Anticoagulation is considered the standard of care for portal vein thrombosis (PVT) in cirrhosis; however, a significant number of patients cannot be safely treated or exhibit thrombus progression despite anticoagulation. We evaluated the role of transjugular intrahepatic portosystemic shunt (TIPS) when indicated exclusively as treatment of PVT in cirrhosis.
Methods
A retrospective study was conducted including all cirrhotic patients with nontumoral PVT treated with TIPS in a tertiary care center. Patients with PVT and additional indications for TIPS were excluded. Feasibility, safety, and efficacy were analyzed. TIPS outcomes compared with a contemporary cohort of patients with TIPS indicated for refractory ascites.
Results
A total of 243 patients were treated by TIPS during the study period, 30 of whom underwent the procedure solely to achieve portal vein recanalization. Portal cavernoma was present in 40% of patients, and 53% of the patients had Yerdel 3 or 4 PVT. Main indications for TIPS were contraindication (53%) or a lack of response (30%) to anticoagulant therapy. In 17% of cases, TIPS was indicated to facilitate liver transplantation (LT) when PVT precluded portal anastomosis. TIPS was successful in 96.6% of patients. Major complications (2 patients) and shunt-related events after TIPS were similar to those reported in the control group. Seventeen percent of patients showed TIPS dysfunction (all successfully treated), a rate similar to that reported in patients with refractory ascites. A higher post-TIPS portacaval pressure gradient was associated with a greater risk of dysfunction. The main portal vein trunk remained patent in all patients, 8 of whom received uneventful LT.
Conclusion
TIPS can be safely performed in patients with cirrhosis and PVT, with an indication for recanalization if medical therapy has failed or is contraindicated.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Clinical and Experimental Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.90
自引率
16.70%
发文量
537
审稿时长
64 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


