全身外源性孕激素加或不加雌激素与静脉曲张手术率降低有关。
IF 2.8
2区 医学
Q2 PERIPHERAL VASCULAR DISEASE
Journal of vascular surgery. Venous and lymphatic disorders
Pub Date : 2025-03-20
DOI:10.1016/j.jvsv.2025.102235
引用次数: 0
摘要
目的:静脉曲张(VV)的危险因素,如女性、妊娠和肥胖是高雌激素状态,但系统性孕激素加或不加雌激素(SPE)在VV治疗中的作用尚未得到很好的描述。本研究探讨了SPE的使用如何影响VV患者的静脉手术率。方法:在TriNetX数据库中查询ICD-10诊断为无症状VV、慢性静脉功能不全和并发VV(炎症、溃疡)的受试者。患者被分为未使用SPE的对照队列、仅使用黄体酮的队列和雌激素-黄体酮联合(CEP)队列。根据VV症状和绝经前状态(年龄)进一步分层结果:数据库查询得到674838名对照组,7597名CEP患者和13758名仅使用黄体酮的患者。经过倾向匹配后,与对照组相比,CEP组接受的刺伤静脉切除术更少(RR=0.52, 95% CI 0.42-0.64)。结论:这项基于人群的大型队列研究表明,尽管雌激素-黄体酮和单孕激素治疗组的DVT和妊娠风险不同,但两种SPE治疗组的VV静脉手术明显少于对照组,单孕激素治疗组接受的静脉手术最少。这需要进一步研究SPE在VV疾病进展中的作用以及全身孕激素作为VV辅助治疗的效用。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Systemic exogenous progestins with or without estrogens are associated with decreased rates of venous procedures for varicose veins
Objectives
Risk factors for varicose veins (VVs) such as female sex, pregnancy, and obesity are high estrogen states, yet the role of systemic progestins with or without estrogens (SPEs) in VV management is not well characterized. This study investigates how SPE use affects rates of venous procedures for patients with VV.
Methods
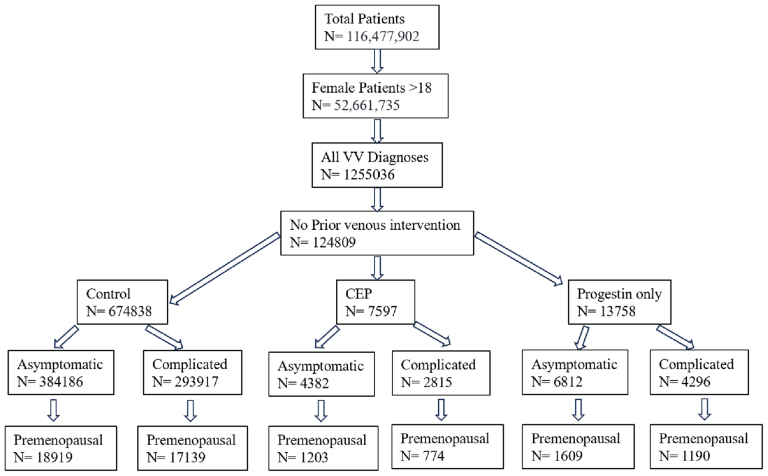
The TriNetX database was queried for subjects with International Classification of Diseases, 10th edition, diagnoses of asymptomatic VV, chronic venous insufficiency, and complicated VV (inflammation or ulceration). Patients were divided into a control cohort with no subsequent SPE use, a progestin-only cohort, and a combined estrogen-progestin (CEP) cohort. Further stratification by VV symptomology and premenopausal status (age <40 years) was also performed. Cohorts were one:one propensity matched on known and theorized risk factors for VV including age, race, prior pregnancy, and body mass index. The outcomes of interest were deep vein thrombosis, pregnancy, stab phlebectomy, endovenous ablation, and sclerotherapy.
Results
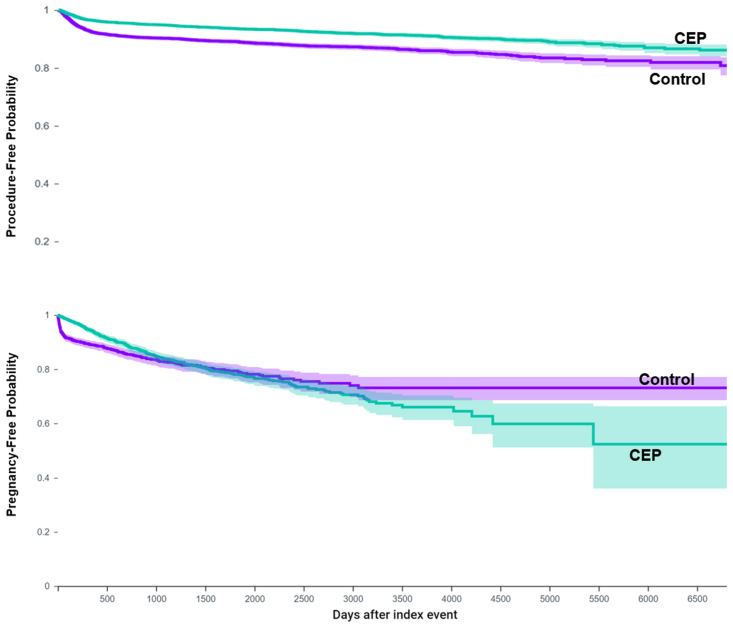
Database query yielded 674,838 controls, 7597 CEP patients, and 13,758 progestin-only patients before matching. After propensity matching, compared with controls, the CEP cohort received fewer stab phlebectomies (relative risk [RR], 0.52; 95% confidence interval [CI], 0.42-0.64; P < .001), endovenous ablations (RR, 0.50; 95% CI, 0.43-0.59; P < .001) or any venous interventions (RR, 0.68; 95% CI, 0.61-0.76; P < .001), with no difference in sclerotherapy (P = .12). Similarly, the progestin-only cohort was less likely to receive stab phlebectomy (RR, 0.37; 95% CI, 0.31-0.43; P < .001), endovenous ablation (RR, 0.35; 95% CI, 0.31-0.40; P < .001), sclerotherapy (RR, 0.65; 95% CI, 0.56-0.75; P < .001), and any venous procedure (RR, 0.57; 95% CI, 0.52-0.62; P < .001). Compared with the progestin-only cohort, the CEP cohort had higher rates of sclerotherapy (RR, 1.38; 95% CI, 1.12-1.72; P = .003) and overall venous procedures (RR, 1.16; 95% CI, 1.00-1.34; P = .048). When possible, analysis stratified by symptomatic status and menopausal status revealed similar findings for subcohorts. Finally, the CEP cohort had lower risk of pregnancy than controls during the first 1200 days of observation, but subsequently had greater risk of pregnancy (RR, 1.38; 95% CI, 1.21-1.57; P < .001). Kaplan-Meier analysis showed that the rates of venous intervention were lower throughout the observation period.
Conclusions
This large, population-based cohort study demonstrated that, despite variable risk of deep vein thrombosis and pregnancy for estrogen-progestin and progestin-only treatment cohorts, both SPE formulations were associated with significantly fewer venous procedures for VVs than controls, with progestin-only cohorts undergoing the fewest procedures. This warrants further investigation into the role of SPE in VV disease progression and the utility of systemic progestins as an adjunct therapy for VVs.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of vascular surgery. Venous and lymphatic disorders
SURGERYPERIPHERAL VASCULAR DISEASE&n-PERIPHERAL VASCULAR DISEASE
CiteScore
6.30
自引率
18.80%
发文量
328
审稿时长
71 days
期刊介绍:
Journal of Vascular Surgery: Venous and Lymphatic Disorders is one of a series of specialist journals launched by the Journal of Vascular Surgery. It aims to be the premier international Journal of medical, endovascular and surgical management of venous and lymphatic disorders. It publishes high quality clinical, research, case reports, techniques, and practice manuscripts related to all aspects of venous and lymphatic disorders, including malformations and wound care, with an emphasis on the practicing clinician. The journal seeks to provide novel and timely information to vascular surgeons, interventionalists, phlebologists, wound care specialists, and allied health professionals who treat patients presenting with vascular and lymphatic disorders. As the official publication of The Society for Vascular Surgery and the American Venous Forum, the Journal will publish, after peer review, selected papers presented at the annual meeting of these organizations and affiliated vascular societies, as well as original articles from members and non-members.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


