初步射频消融与聚多坎醇微泡沫消融治疗有症状、功能不全的小隐静脉的早期疗效比较。
IF 2.8
2区 医学
Q2 PERIPHERAL VASCULAR DISEASE
Journal of vascular surgery. Venous and lymphatic disorders
Pub Date : 2025-03-20
DOI:10.1016/j.jvsv.2025.102234
引用次数: 0
摘要
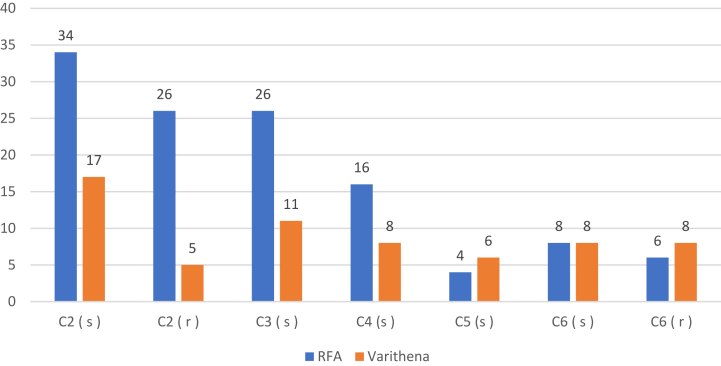
背景:临床实践指南支持射频消融术(RFA)治疗有症状、功能不全的小隐静脉(SSV),但由于缺乏高质量的临床数据,这些指南并未涉及聚多卡因醇微泡沫消融术(MFA)。然而,与RFA相比,使用MFA时,SSV反流患者的一些解剖变异和临床情况可能与相同或更好的结果相关。本研究旨在比较使用RFA或MFA治疗CEAP 2-6疾病患者SSV功能不全后的早期结果。方法:对接受RFA或MFA治疗的不合格ssv患者的前瞻性数据库进行回顾性评价。同时行静脉切除术的肢体包括在内。所有患者术后48-72小时接受双超声检查,并由血管外科医生进行至少一次随访。主要结果是SSV立即关闭和消融相关血栓延伸(ARTE)。次要结果分析包括人口统计数据、CEAP临床分类、静脉临床严重程度评分(VCSS)、深静脉血栓形成(DVT)和不良事件。结果:在2018年3月至2024年7月期间,182名ssv患者接受了RFA (n=120)或MFA (n=62)的症状性反流治疗。两组的年龄、性别、体重指数、反流次数和SSV直径相似。RFA组术前VCSS平均值为9.4 + 3.0,MFA组术前VCSS平均值为10.8 + 3.7,差异有统计学意义(p=0.05)。MFA时静脉溃疡发生率(n=16, 26%)高于RFA (n=14, 12%) (p=0.015)。RFA组中位随访时间为164.5天,MFA组中位随访时间为156天。RFA和MFA后症状改善率分别为91%和88%。RFA组术后平均VCSS从9.4降至7.3。结论:RFA和MFA对于有症状、功能不全的SSV患者均是安全有效的治疗方法。两种方法均获得了良好的临床缓解和早期截静脉关闭率。MFA组溃疡愈合的数量更高,但这种差异仅在单变量分析中是显著的。RFA后的不良血栓事件很低,与其他当代研究一致,尽管MFA后的浅表性静脉炎更常见。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Comparative early outcomes following primary radiofrequency ablation and polidocanol microfoam ablation of symptomatic, incompetent small saphenous veins
Background
Radiofrequency ablation (RFA) of symptomatic, incompetent small saphenous veins (SSVs) is supported by clinical practice guidelines, but polidocanol microfoam ablation (MFA) is not addressed in these guidelines owing to the absence of high-quality clinical data. However, some anatomical variations and clinical scenarios in patients with SSV reflux may be associated with equivalent or superior results when MFA is used compared with RFA. This study aims to compare early outcomes after the treatment of SSV incompetence in patients with Clinical-Etiology-Anatomy-Pathophysiology (CEAP) 2 class to 6 disease using either RFA or MFA.
Methods
A retrospective review of a prospectively maintained database was conducted among patients who underwent treatment of incompetent SSVs with either RFA or MFA. Limbs that underwent concomitant phlebectomy were included. All patients underwent postoperative duplex ultrasound at 48 to 72 hours and at least one follow-up visit by a vascular surgery provider. Primary outcomes were immediate SSV closure and ablation-related thrombus extension. Secondary outcomes analyzed included demographic data, CEAP clinical class, Venous Clinical Severity Score (VCSS), deep venous thrombosis, and adverse events.
Results
Between March 2018 and July 2024, 182 SSVs treated for symptomatic reflux with either RFA (n = 120) or MFA (n = 62) were identified. Age, gender, body mass index, reflux times, and SSV diameters were similar between both groups. The mean preoperative VCSSs were 9.4 ± 3.0 and 10.8 ± 3.7 in the RFA and MFA groups, respectively (P = .05). More venous ulcers were present at the time of MFA (n = 16 [26%]) than RFA (n = 14 [12%]) (P = .015). Median follow-up was 164.5 days in the RFA cohort and 156 days after MFA. Symptomatic improvement after RFA and MFA was 91% and 88%, respectively. The mean postoperative VCSS decreased from 9.4 to 7.3 in the RFA group (P < .001) and from 10.9 to 9.2 after MFA (P < .001). Immediate vein closure was achieved in 98% of limbs in both groups; two late recanalizations occurred after MFA, but none after RFA. The number of ulcers healed at last follow-up was greater after MFA (n = 13 [81%] vs n = 10 [71%]; P = .02). The incidence of ablation-related thrombus extension was 4.8% (n = 3) after MFA and 1.7% (n = 2) after RFA (P = .52). One gastrocnemius deep venous thrombosis occurred in the MFA group. No pulmonary emboli or central nervous complications occurred. All adverse thrombotic events were asymptomatic and resolved with short-term anticoagulation. Superficial phlebitis was higher after MFA (n = 11 [17.7%] vs n = 5 [4.2%]; P = .002) One postoperative sural neuralgia occurred after RFA.
Conclusions
RFA and MFA are both safe and effective treatments for patients with symptomatic, incompetent SSVs. Both resulted in excellent clinical relief and early truncal vein closure rates. The number of ulcers healed was higher in the MFA group, but this difference was significant on univariate analysis only. Adverse thrombotic events after RFA were low and consistent with other contemporary studies, although superficial phlebitis was more frequent after MFA.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of vascular surgery. Venous and lymphatic disorders
SURGERYPERIPHERAL VASCULAR DISEASE&n-PERIPHERAL VASCULAR DISEASE
CiteScore
6.30
自引率
18.80%
发文量
328
审稿时长
71 days
期刊介绍:
Journal of Vascular Surgery: Venous and Lymphatic Disorders is one of a series of specialist journals launched by the Journal of Vascular Surgery. It aims to be the premier international Journal of medical, endovascular and surgical management of venous and lymphatic disorders. It publishes high quality clinical, research, case reports, techniques, and practice manuscripts related to all aspects of venous and lymphatic disorders, including malformations and wound care, with an emphasis on the practicing clinician. The journal seeks to provide novel and timely information to vascular surgeons, interventionalists, phlebologists, wound care specialists, and allied health professionals who treat patients presenting with vascular and lymphatic disorders. As the official publication of The Society for Vascular Surgery and the American Venous Forum, the Journal will publish, after peer review, selected papers presented at the annual meeting of these organizations and affiliated vascular societies, as well as original articles from members and non-members.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


