淋巴小体四切口淋巴小囊吻合治疗下肢淋巴水肿的疗效研究。
IF 2.8
2区 医学
Q2 PERIPHERAL VASCULAR DISEASE
Journal of vascular surgery. Venous and lymphatic disorders
Pub Date : 2025-03-03
DOI:10.1016/j.jvsv.2025.102221
引用次数: 0
摘要
背景:下肢淋巴水肿(LLL)是一种慢性淋巴排水受损的疾病。淋巴小静脉吻合术(LVA)是一种很有前途的显微外科治疗方法。精细的手术技术,如最佳切口位置和精确的淋巴管识别,对于更好的临床结果至关重要。目的:经淋巴小体四切口入路行淋巴-小静脉吻合。规范切口定位,明确LVA的淋巴管,提高手术效果。方法:对59例LLL行LVA的患者进行回顾性研究。其中研究组32例采用四切口入路行LVA,对照组27例采用经验确定切口位置行LVA。术后随访12个月。结果测量包括淋巴-静脉吻合术数量、手术时间、淋巴水肿功能、残疾、下肢淋巴水肿健康问卷(淋巴- icf)和下肢淋巴水肿指数(LELI)、患者健康问卷-9项(PHQ-9)和皮下厚度。结果:随访6个月和12个月时,两组患者在LELI和淋巴细胞增殖因子方面存在显著的交互作用(P < 0.05)。两组间PHQ-9无交互作用(P < 0.05)。治疗后,研究组皮下厚度明显低于对照组(P < 0.05)。两组手术时间及淋巴-静脉吻合术个数比较,差异无统计学意义(P < 0.05)。结论:经淋巴体为基础的四切口入路LVA可显著提高LLL患者的生活质量、肢体体积和皮下厚度。本研究提出了新的LVA切口选择标准,强调了综合考虑患者心理健康的必要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Efficacy study of lymphaticovenular anastomosis via the lymphosome-based four-incision approach for lower limb lymphedema
Objective
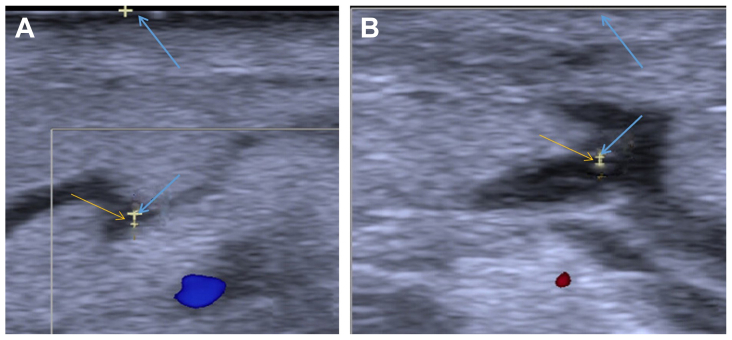
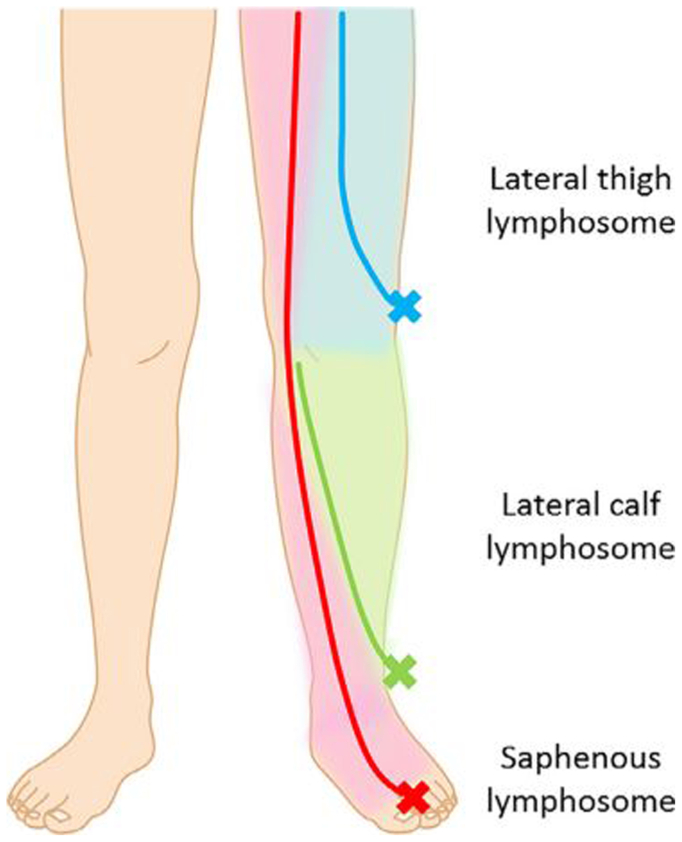
Lower limb lymphedema (LLL) is a chronic condition with impaired lymphatic drainage. Lymphaticovenular anastomosis (LVA) is a promising microsurgical treatment for LLL. Refined surgical techniques, such as optimal incision placement and precise lymphatic vessel identification, are essential for better clinical outcomes. For patients with LLL, we performed an LVA via the lymphosome-based four-incision approach. We standardized incision positioning and identified lymphatic vessels for LVA to improve surgical outcomes.
Methods
A retrospective study was conducted on 59 patients with LLL who underwent LVA. Among them, 32 patients in the study group received LVA using the four-incision approach, and 27 patients in the control group underwent LVA with empirically determined incision placement. All patients were followed up for 12 months after the operation. The outcome measures included the number of lymphatic-to-venous anastomoses, surgical duration, Lymphedema Functioning, Disability, and Health Questionnaire for Lower Limb Lymphedema and Lower Extremity Lymphedema Index, Patient Health Questionnaire-9 items, and subcutaneous thickness.
Results
At the 6-month and 12-month follow-ups, there was a significant interaction between the two groups of patients in terms of Lower Extremity Lymphedema Index and Lymphedema Functioning, Disability, and Health Questionnaire for Lower Limb Lymphedema (P < .05). The Patient Health Questionnaire-9 items showed no interaction between the two groups (P > .05). After treatment, the subcutaneous thickness in the study group was lower than that in the control group (P < .05). There were no significant differences between the two groups regarding surgical duration and the number of lymphatic-to-venous anastomoses (P > .05).
Conclusions
LVA via the lymphosome-based four-incision approach can significantly enhance the quality of life, limb volume, and subcutaneous thickness in patients with LLL. This study presents new incision selection criteria for LVA and underlines the necessity of comprehensively addressing patients’ mental health.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of vascular surgery. Venous and lymphatic disorders
SURGERYPERIPHERAL VASCULAR DISEASE&n-PERIPHERAL VASCULAR DISEASE
CiteScore
6.30
自引率
18.80%
发文量
328
审稿时长
71 days
期刊介绍:
Journal of Vascular Surgery: Venous and Lymphatic Disorders is one of a series of specialist journals launched by the Journal of Vascular Surgery. It aims to be the premier international Journal of medical, endovascular and surgical management of venous and lymphatic disorders. It publishes high quality clinical, research, case reports, techniques, and practice manuscripts related to all aspects of venous and lymphatic disorders, including malformations and wound care, with an emphasis on the practicing clinician. The journal seeks to provide novel and timely information to vascular surgeons, interventionalists, phlebologists, wound care specialists, and allied health professionals who treat patients presenting with vascular and lymphatic disorders. As the official publication of The Society for Vascular Surgery and the American Venous Forum, the Journal will publish, after peer review, selected papers presented at the annual meeting of these organizations and affiliated vascular societies, as well as original articles from members and non-members.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


