近视与糖尿病视网膜病变之间的关系:一项双样本孟德尔随机研究。
IF 3.4
Advances in ophthalmology practice and research
Pub Date : 2025-02-01
DOI:10.1016/j.aopr.2024.10.003
引用次数: 0
摘要
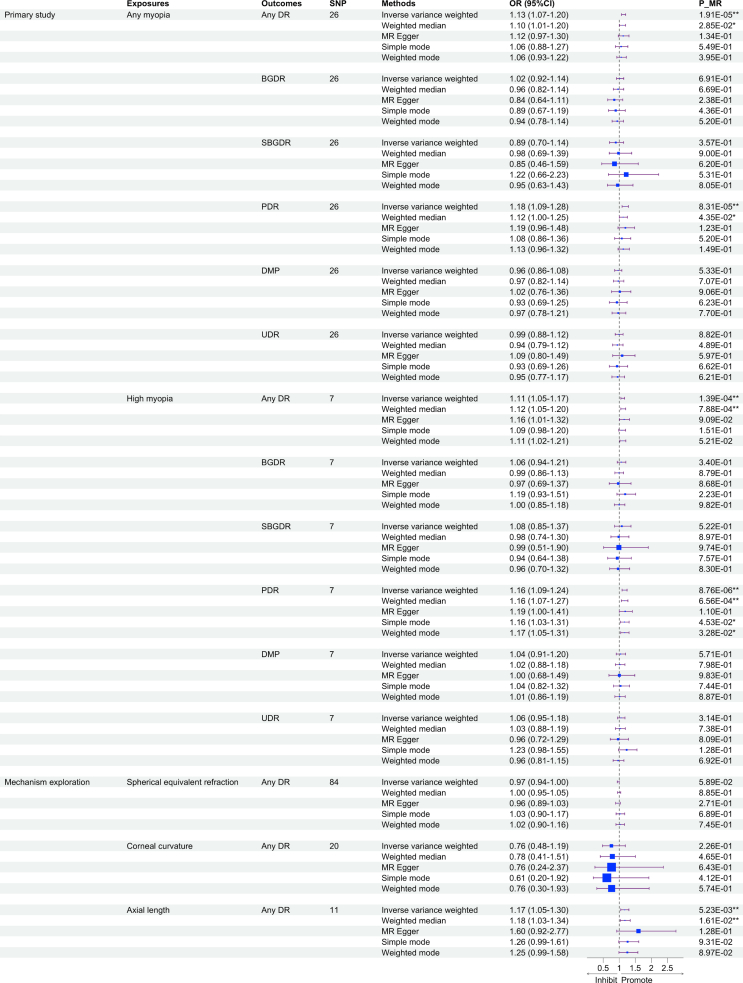
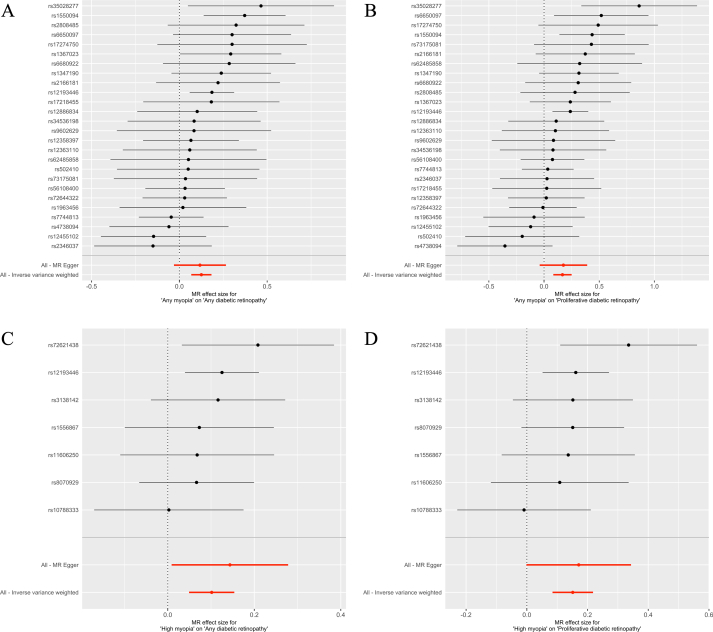
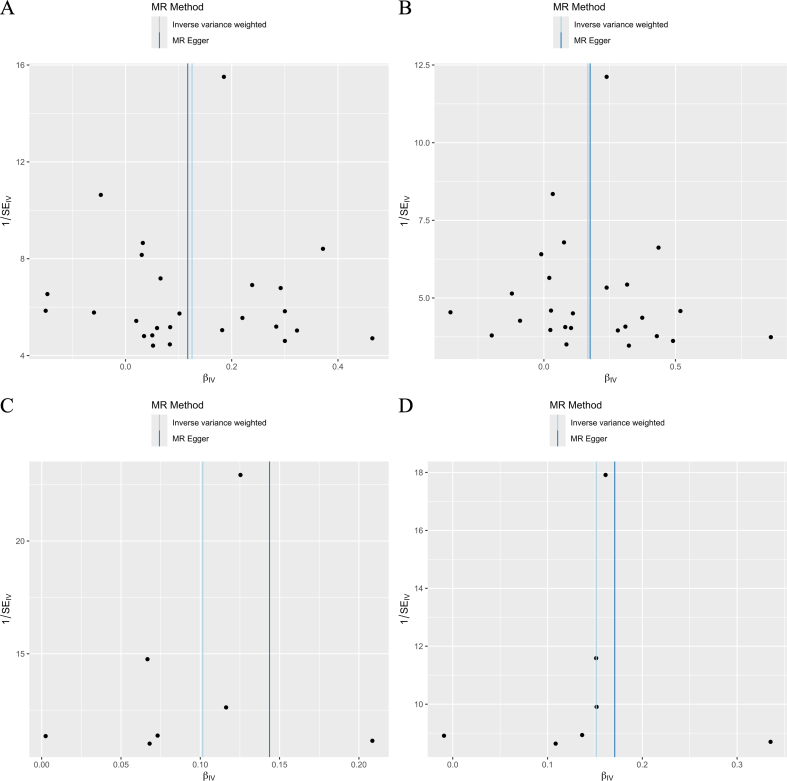
目的:近视与糖尿病视网膜病变(DR)之间的关系尚不清楚,报道的结果不一致,这种关系是否代表因果关系尚不清楚。本研究旨在探讨遗传性近视与DR的因果关系,并进一步探讨其具体机制。方法:本研究采用双样本孟德尔随机化(MR)方法对任意近视和高度近视6种DR表型进行分析,包括任意DR、背景DR、重度背景DR、增殖性DR、糖尿病黄斑病变和非特异性DR。随后对任意DR的球面等效折射(SER)、角膜曲率(CC)和轴向长度(AL)进行了机理探索。单核苷酸多态性(snp)作为遗传工具,来源于UK Biobank、英国成人健康与衰老队列遗传流行病学研究(GERA)和FinnGen。因果关系评价主要采用反方差加权法(IVW),并辅以敏感性分析和因果关系方向分析。结果:使用排除了可能混杂因素的snp,我们发现任何近视与任何DR (IVW:比值比[OR] = 1.133, 95%可信区间[95%CI]: 1.070-1.201, P = 1.91×10-5)和PDR (IVW: OR = 1.182, 95%CI: 1.088-1.285, P = 8.31×10-5)之间存在暗示和正相关的因果关系。高度近视与任何DR和PDR均有相似但更显著的相关性(IVW: OR = 1.107, 95%CI: 1.051 ~ 1.166, P = 1.39×10-4;或= 1.163,95%置信区间ci: 1.088 - -1.244, P = 8.76×10 - 6,分别)。进一步的机制分析发现,只有AL,而不是SER或CC,与任何dr都有强烈而显著的相关性。这些相关性在敏感性分析和因果关系方向分析中都是稳健的。结论:我们发现任何近视和高度近视与DR和PDR的风险均存在显著正相关的因果关系,这可能与AL有关,说明控制近视对预防DR的发生和发展具有重要意义。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Association between myopia and diabetic retinopathy: A two-sample mendelian randomization study
Objective
The association between myopia and diabetic retinopathy (DR) is unclear, with inconsistent results reported, and whether the association represents causality remains unknown. This study aimed to investigate the causal associations of genetically determined myopia with DR, and further explore specific mechanisms.
Methods
We conducted two-sample mendelian randomization (MR) analyses of any myopia and high myopia on six DR phenotypes, including any DR, background DR, severe background DR, proliferative DR (PDR), diabetic maculopathy and unspecific DR in the primary study. Mechanism exploration of spherical equivalent refraction (SER), corneal curvature (CC) and axial length (AL) on any DR was carried out subsequently. Single-nucleotide polymorphisms (SNPs), used as genetic instruments, were derived from UK Biobank, Genetic Epidemiology Research on Adult Health and Aging cohort (GERA) and FinnGen. The inverse variance weighted (IVW) method was mainly used to assess the causality, and was complemented with sensitivity analyses and causality direction analyses.
Results
Using SNPs that have excluded possible confounders, we discovered suggestive and positive causal associations of any myopia with any DR (IVW: odds ratio [OR] = 1.133, 95% confidence interval [95%CI]: 1.070–1.201, P = 1.91×10−5) and PDR (IVW: OR = 1.182, 95% CI: 1.088–1.285, P = 8.31×10−5). Similar but more significant associations were found of high myopia with any DR and PDR (IVW: OR = 1.107, 95%CI: 1.051–1.166, P = 1.39×10−4; OR = 1.163, 95%CI: 1.088–1.244, P = 8.76×10−6, respectively). Further mechanism analyses found only AL, rather than SER or CC, was strongly and significantly associated with any DR. These associations were robust in sensitivity analyses and causality direction analyses.
Conclusions
We found significant and positive causal associations of any myopia and high myopia with the risk of DR and PDR, which might be related with AL, indicating the significance of myopia control for preventing DR development and progression.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Advances in ophthalmology practice and research
Ophthalmology
CiteScore
1.70
自引率
0.00%
发文量
0
审稿时长
66 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


