恶性副神经节瘤伴头颅转移,表现为复发性儿茶酚胺引起的心肌病。
IF 1.2
Q3 Medicine
引用次数: 0
摘要
背景/目的:头颅转移很少发生在恶性副神经节瘤(PGLs)或嗜铬细胞瘤中,它们通常转移到肝脏、骨骼、肺和淋巴结。考虑到关键位置,采用多学科方法进行早期发现和干预至关重要。病例报告:我们的患者是一名31岁的男性,9岁时被诊断为主动脉周围PGL和琥珀酸脱氢酶亚基B致病性变异,并伴有心脏骤停。他在14岁时患上了腹腔和骨骼转移性疾病,并接受了手术、化疗和放疗。失访后,患者紧急出现头痛、心悸、高血压危像、2型非st段抬高型心肌梗死、儿茶酚胺性心肌病,血浆游离肾上腺素61.0 pg/mL (0.0 ~ 88.0 pg/mL),血清游离去甲肾上腺素662.9 pg/mL (0.0 ~ 210.1 pg/mL)升高。影像学显示右额颅病变,颅内硬脑膜内4.9 cm,颅外4.9 cm,枕骨病变1.5 cm。肾上腺素能阻断后,患者行额叶病变切除术,病理显示转移性PGL。讨论:咨询了多学科团队。由于潜在的神经毒性,放射学建议不要进行放射治疗。肿瘤学建议监测。术后7个月,镓-68十二烷四乙酸-奥醋酸正电子发射断层扫描/计算机断层扫描显示手术部位无复发,枕部病变稳定,并有额外的骨骼转移。计划对患者进行肽受体放射性核素治疗。结论:本病例强调了主动监测PGL和嗜铬细胞瘤的重要性,以便对转移性疾病进行早期干预,并回顾了有争议的罕见颅骨或脑转移治疗,包括肽受体放射性核素治疗。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Malignant Paraganglioma With Calvarial Metastases Presenting With Recurrent Catecholamine-Induced Cardiomyopathy
Background/Objective
Cranial metastases rarely occur in malignant paragangliomas (PGLs) or pheochromocytomas, which usually metastasize to the liver, bone, lungs, and lymph nodes. Early detection and intervention with a multidisciplinary approach are crucial given the critical location.
Case Report
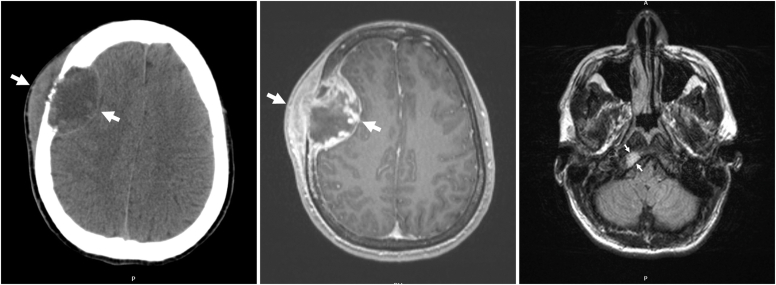
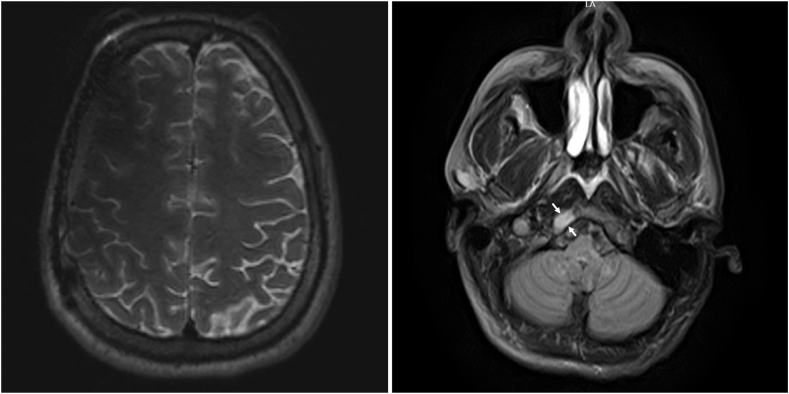
Our patient was a 31-year-old man diagnosed with periaortic PGL and succinate dehydrogenase subunit B pathogenic variant at the age of 9 years with cardiac arrest. He developed intra-abdominal and skeletal metastatic disease by the age of 14 years and treated with surgery, chemotherapy, and radiation. After being lost to follow-up, the patient presented emergently with headache, palpitations, hypertensive crisis, type 2 non-ST-elevation myocardial infarction, and catecholamine-induced cardiomyopathy, with plasma free metanephrine level of 61.0 pg/mL (0.0-88.0 pg/mL) and elevated serum free normetanephrine level of 662.9 pg/mL (0.0-210.1 pg/mL). Imaging showed a right frontal calvarial lesion, with 4.9-cm intracranial dural and 4.9-cm extracranial components, and a 1.5-cm occipital bone lesion. Following adrenergic blockade, the patient underwent resection of the frontal lesion with pathology showing metastatic PGL.
Discussion
A multidisciplinary team was consulted. Because of potential neurotoxicity, radiology advised against radiotherapy. Oncology advised monitoring. Seven months postoperatively, gallium-68 dodecane tetraacetic acid–octreotate positron emission tomography/computed tomography showed no recurrence at the surgical site, stable occipital lesion, and additional skeletal metastases. The patient is planned for peptide receptor radionuclide therapy.
Conclusion
Our case highlights the importance of active surveillance in PGL and pheochromocytoma to allow early intervention for metastatic disease and reviews the controversial management of rare calvarial or cerebral metastases, including peptide receptor radionuclide therapy.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

AACE Clinical Case Reports
Medicine-Endocrinology, Diabetes and Metabolism
CiteScore
2.30
自引率
0.00%
发文量
61
审稿时长
55 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


