伴血浆肾上腺素水平增高的嗜铬细胞-神经节神经瘤2例。
IF 1.2
Q3 Medicine
引用次数: 0
摘要
背景/目的:病例报告:患者1和患者2分别为35岁和45岁的女性。患者1有高血压控制史,焦虑症状伴心悸、出汗和潮红。患者2主诉腹痛,行腹部计算机断层扫描(CT)。患者1和患者2的肾上腺素水平分别为76 pg/mL和61 pg/mL(正常)。讨论:嗜铬细胞瘤-神经节神经瘤的临床和影像学表现反映了嗜铬细胞瘤。诊断依赖于组织病理学分析。嗜铬细胞-神经节神经瘤的治疗是在肾上腺专业的高容量中心进行完全手术切除,总体预后良好。复发率低,远端转移很少报道。结论:嗜铬细胞-神经节神经瘤可能在亚临床范围内存在血浆肾上腺素水平。与分离的嗜铬细胞瘤一样,终生监测对复合嗜铬细胞瘤-神经节神经瘤至关重要。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Two Cases of Composite Pheochromocytoma-Ganglioneuromas With Plasma Metanephrine Levels in the Subclinical Range Pheochromocytoma-Ganglioneuroma
Background/Objective
In <10% of cases, pheochromocytomas coexist with other tumors, most commonly ganglioneuromas, and are termed composite pheochromocytoma-ganglioneuromas. We present 2 cases of composite pheochromocytoma-ganglioneuromas and review the diagnosis and management of these rare tumors.
Case Report
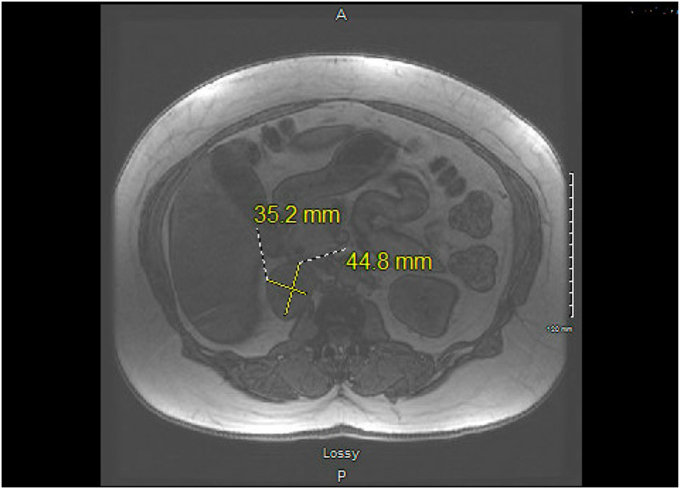
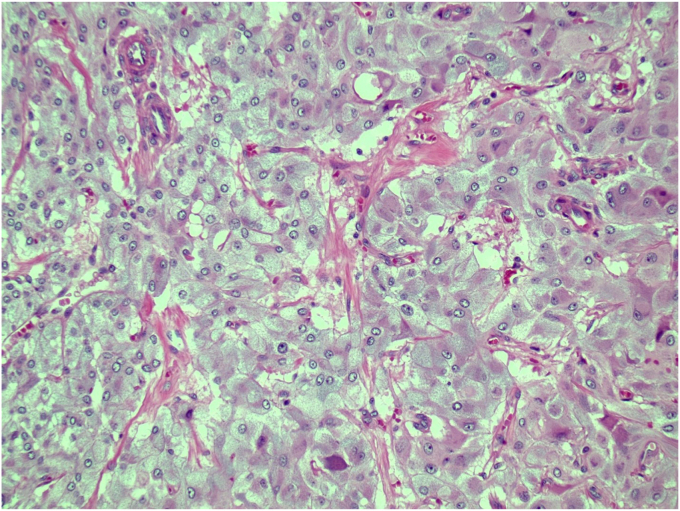
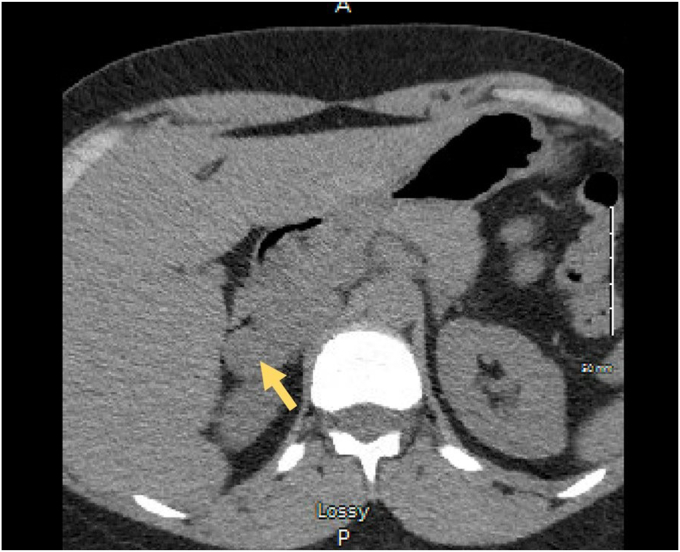
Patient 1 and patient 2 were 35-year-old and 45-year-old woman, respectively. Patient 1 presented with a history of controlled hypertension and symptoms of anxiety along with palpitations, diaphoresis, and flushing. Patient 2 complained of abdominal pain and underwent abdominal computed tomography (CT) imaging. Patient 1 and patient 2 had metanephrine levels of 76 pg/mL and 61 pg/mL (normal <57 pg/mL), respectively, and normetanephrine levels of 161 pg/mL and 116 pg/mL (normal < 148 pg/mL), respectively. CT scans depicted right adrenal masses in both cases: patient 1 had a 2.3 × 2.6 cm mass measuring 36 Hounsfield units on noncontrast CT imaging and patient 2 had a 4.5 × 3.5 cm right adrenal mass measuring 73 Hounsfield units on contrast CT imaging. Both patients underwent laparoscopic robotic adrenalectomies without complications. The pathologic analyses of both cases revealed composite pheochromocytoma-ganglioneuroma tumors. Surveillance at 1 year in both patients demonstrated no evidence of recurrence.
Discussion
The clinical and radiological presentation of composite pheochromocytoma-ganglioneuromas mirrors pheochromocytomas. The diagnosis relies on histopathological analysis. Treatment of pheochromocytoma-ganglioneuromas is complete surgical excision in a high-volume center with adrenal expertise and is associated with an overall excellent prognosis. The probability of recurrence is low, and distant metastases have rarely been reported.
Conclusion
Pheochromocytoma-ganglioneuromas may present with plasma metanephrine levels in the subclinical range. As with isolated pheochromocytomas, lifetime surveillance is critical for composite pheochromocytoma-ganglioneuromas.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

AACE Clinical Case Reports
Medicine-Endocrinology, Diabetes and Metabolism
CiteScore
2.30
自引率
0.00%
发文量
61
审稿时长
55 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


