肺癌解剖肺切除术后的意外再手术:在前瞻性多中心数据库中的发生率、危险因素、早期结果和长期预后影响
IF 9.2
3区 医学
Q1 RESPIRATORY SYSTEM
引用次数: 0
摘要
目的:该研究旨在确定肺癌解剖性肺切除术后与非计划再手术(UR)相关的围手术期变量,并调查其对长期预后结果的影响:该研究旨在确定肺癌解剖性肺切除术后与非计划再手术(UR)相关的围手术期变量,并调查其对长期预后结果的影响:回顾性分析了2016年12月至2018年3月在全国范围内前瞻性登记的肺癌解剖性肺切除术患者的记录。进行多变量逻辑回归分析,寻找 UR 的风险因素。比较了短期结果,并计算了院内和90天死亡率的调整后几率比。在平衡基线混杂因素后,采用倾向评分匹配法和对数秩检验评估了UR对总生存期(OS)和无病生存期(DFS)的预后价值:对3085名患者的数据进行了研究,发现UR发病率为4.12%。多变量逻辑回归分析显示,男性性别(OR=3.288,P=0.004)、ppoDLCO%(OR=0.975,P=0.003)、气胸切除术(OR=4.748,P=0.038)、强胸膜粘连(OR=3.449,PConclusion:男性性别、ppoDLCO%、气胸切除术、强胸膜粘连和手术室工作量均与UR独立相关。UR与围手术期死亡率升高有关,但与长期死亡率升高无关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
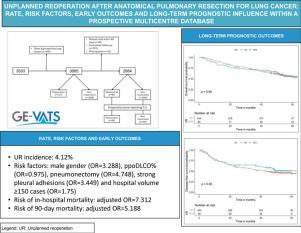
Unplanned Reoperation After Anatomical Pulmonary Resection for Lung Cancer: Rate, Risk Factors, Early Outcomes and Long-term Prognostic Influence Within a Prospective Multicentre Database
Objectives
The study aimed to identify perioperative variables associated with unplanned reoperation (UR) following anatomical pulmonary resection for lung cancer and investigate its impact on long-term prognostic outcomes.
Methods
The records of patients who underwent anatomical pulmonary resection for lung cancer from December 2016 to March 2018 within a nationwide prospective registry were reviewed. Multivariable logistic regression analyses were performed to find the risk factors for UR. The short-term outcomes were compared, and the adjusted odds ratios for in-hospital and 90-day mortality were calculated. The prognostic value of UR for overall survival (OS) and disease-free survival (DFS) was assessed using the Kaplan–Meier method and log-rank test after propensity score matching for balancing baseline confounders.
Results
Data from 3085 patients were examined, revealing a UR incidence of 4.12%. Multivariable logistic regression analyses revealed that male gender (OR = 3.288, P = 0.004), ppoDLCO% (OR = 0.975, P = 0.003), pneumonectomy (OR = 4.748, P = 0.038), strong pleural adhesions (OR = 3.449, P < 0.001) and hospital volume ≥150 cases (OR = 1.75, P = 0.026) were independently associated with UR. Risk of in-hospital and 90-day mortality was higher in UR cases (adjusted OR = 7.312, P < 0.001, and OR = 5.188, P < 0.001, respectively). Ninety-eight UR and 347 matched non-UR cases were included in the long-term follow-up analysis. The median follow-up time was 50.4 months. No significant differences were found in OS, and DFS between groups (log rank P = 0.953 and P = 0.352, respectively).
Conclusion
Male gender, ppoDLCO%, pneumonectomy, strong pleural adhesions, and surgical unit workload were all independently associated with UR. UR was associated with an increased perioperative mortality, but not with a higher long-term mortality.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Archivos De Bronconeumologia
Medicine-Pulmonary and Respiratory Medicine
CiteScore
3.50
自引率
17.50%
发文量
330
审稿时长
14 days
期刊介绍:
Archivos de Bronconeumologia is a scientific journal that specializes in publishing prospective original research articles focusing on various aspects of respiratory diseases, including epidemiology, pathophysiology, clinical practice, surgery, and basic investigation. Additionally, the journal features other types of articles such as reviews, editorials, special articles of interest to the society and editorial board, scientific letters, letters to the editor, and clinical images. Published monthly, the journal comprises 12 regular issues along with occasional supplements containing articles from different sections.
All manuscripts submitted to the journal undergo rigorous evaluation by the editors and are subjected to expert peer review. The editorial team, led by the Editor and/or an Associate Editor, manages the peer-review process. Archivos de Bronconeumologia is published monthly in English, facilitating broad dissemination of the latest research findings in the field.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


