颅骨切除术和颅骨成形术对康复中平衡和步态影响的回顾性研究。
IF 2
Q2 REHABILITATION
Archives of rehabilitation research and clinical translation
Pub Date : 2024-12-01
DOI:10.1016/j.arrct.2024.100375
引用次数: 0
摘要
目的:分析接受颅骨切除术和颅骨成形术后康复的患者平衡和步态的变化,包括不同时间段的结果、变化率和诊断之间的比较。设计:回顾性队列研究。环境:住院康复。参与者:53例患者(平均年龄52.3±16.9岁;(62%男性)在颅骨切除术或颅骨成形术后伴有中风、创伤性或非创伤性脑损伤。干预措施:不适用。主要结果测量:在基线、首次出院、再入院和最终出院时收集Berg平衡量表(BBS)、功能步态评估(FGA)、6分钟步行测试(6MWT)和10米步行测试(10MWT)。结果:在整个康复过程中,所有4项结果均有所改善:BBS, 17.9分(95%可信区间[CI], 12.7-23.2);FGA, 7.8分(95% CI, 0.6-15.0);6MWT, 141.0 m (95% CI, 89.0-192.0);10MWT, 0.381 m/s (95% CI, 0.188-0.575)。所有结果在颅骨切除术后入院时均有改善:BBS, 13.0分(95% CI, 8.4-17.5);FGA, 4.0点(95% CI)。-1.65 - 9.65);6MWT, 100.0 m (95% CI, 58.2-142.0);10MWT为0.160 m/s (95% CI, 0.004-0.316)。在康复休假期间,BBS下降6.3分(95% CI, -11.8至-0.8);FGA下降6.6点(95% CI, -13.8至0.6);6MWT降低19.2 m (95% CI, -73.5 ~ 35.2);10MWT增加0.089 m/s (95% CI, -0.097 ~ 0.276)。颅骨成形术后入院时所有结果均有改善:BBS, 11.3分(95% CI, 6.6-16.0);FGA, 10.4点(95% CI, 4.8-16.1);6MWT, 59.4 m (95% CI, 14.1-105.0);10MWT为0.132 m/s (95% CI, -0.039 ~ 0.303)。诊断与结果的改变无关。结论:步态和平衡结果在颅骨切除术和颅骨成形术后康复入院期间有所改善,但在颅骨成形术后没有立即改善。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Craniectomy and Cranioplasty Effects on Balance and Gait in Rehabilitation: A Retrospective Study
Objective
To analyze changes in balance and gait in patients undergoing rehabilitation postcraniectomy and postcranioplasty, including comparison of outcomes across time periods, rate of change, and among diagnoses.
Design
Retrospective cohort study.
Setting
Inpatient rehabilitation.
Participants
Fifty-three patients (mean age 52.3±16.9y; 62% male) with stroke, traumatic, or nontraumatic brain injury postcraniectomy or postcranioplasty.
Interventions
Not applicable.
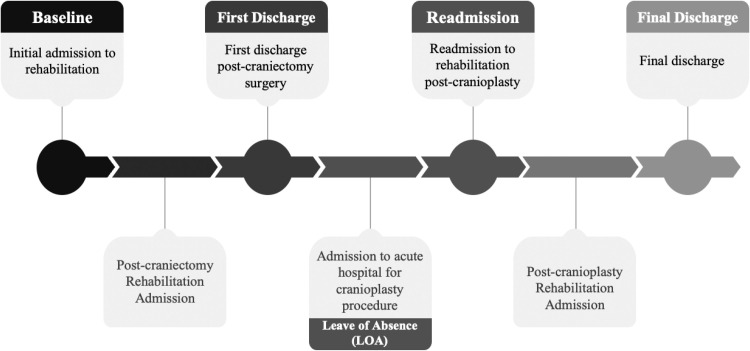
Main Outcome Measures
Berg Balance Scale (BBS), Functional Gait Assessment (FGA), 6-minute walk test (6MWT), and 10-meter walk test (10MWT) were collected at baseline, first discharge, readmission, and final discharge.
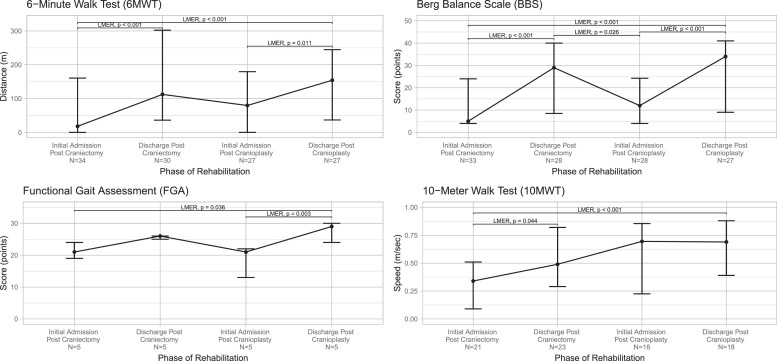
Results
Across the full rehabilitation course, all 4 outcomes improved: BBS, 17.9 points (95% confidence interval [CI], 12.7-23.2); FGA, 7.8 points (95% CI, 0.6-15.0); 6MWT, 141.0 m (95% CI, 89.0-192.0); and 10MWT, 0.381 m/s (95% CI, 0.188-0.575). All outcomes improved at postcraniectomy admission: BBS, 13.0 points (95% CI, 8.4-17.5); FGA, 4.0 points (95% CI. −1.65 to 9.65); 6MWT, 100.0 m (95% CI, 58.2-142.0); and 10MWT, 0.160 m/s (95% CI, 0.004-0.316). During leave of absence from rehabilitation, BBS decreased 6.3 points (95% CI, −11.8 to −0.8); FGA decreased 6.6 points (95% CI, −13.8 to 0.6); 6MWT decreased 19.2 m (95% CI, −73.5 to 35.2); and 10MWT increased 0.089 m/s (95% CI, −0.097 to 0.276). All outcomes improved at postcranioplasty admission: BBS, 11.3 points (95% CI, 6.6-16.0); FGA, 10.4 points (95% CI, 4.8-16.1); 6MWT, 59.4 m (95% CI, 14.1-105.0); and 10MWT, 0.132 m/s (95% CI, −0.039 to 0.303). Diagnosis was not associated with changes in outcomes.
Conclusions
Gait and balance outcomes improved during postcraniectomy and postcranioplasty rehabilitation admissions but not immediately post cranioplasty.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Archives of rehabilitation research and clinical translation
Medicine and Dentistry (General)
CiteScore
3.00
自引率
0.00%
发文量
0
审稿时长
8 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


