成人获得性脑损伤住院康复中功能恢复率与治疗时间和内容的关系。
IF 2
Q2 REHABILITATION
Archives of rehabilitation research and clinical translation
Pub Date : 2024-12-01
DOI:10.1016/j.arrct.2024.100370
引用次数: 0
摘要
目的:探讨成人后发性脑损伤患者康复治疗的时间和内容与自我护理和活动功能恢复率的关系。设计:回顾性队列研究,使用电子健康记录和行政账单数据。环境:在一个大型学术医疗中心的住院康复单位。参与者:2012年至2017年住院康复病房的原发性诊断为中风、创伤性脑损伤或非创伤性脑损伤的成年人(N=799)。干预措施:不适用。主要结果测量:自理和活动功能的获得率,使用功能独立性测量。使用层次回归模型来确定基线特征、单位和职业治疗、物理治疗和语言病理治疗的内容对功能增益率的贡献。结果:康复时间中位数为10天(四分位数间8-13天)。患者平均每天接受10.62个单位的治疗(SD, 2.05)。对于自我保健护理增益率,最佳拟合模型占方差的32%。日常生活单位的职业治疗活动与增重率呈正相关。对于流动性增益率,最佳拟合模型占方差的37%。高强度的床上活动能力训练与活动能力增加率呈负相关。结论:在职业治疗中,更多的日常生活活动与获得性脑损伤成人自我保健功能的更快改善有关,而在物理治疗中,更多的床上活动与较慢的改善有关。基于价值的支付的一个潜在挑战是临床适当的治疗活动与评估患者改善的指标之间的一致性。有一种风险是,治疗师和医疗机构会优先考虑推动指标改善的活动,而忽视其他以患者为中心的目标。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Association of Rate of Functional Recovery With Therapy Time and Content Among Adults With Acquired Brain Injuries in Inpatient Rehabilitation
Objective
To examine associations among the time and content of rehabilitation treatment with self-care and mobility functional gain rate for adults with acquired brain injury.
Design
Retrospective cohort study using electronic health record and administrative billing data.
Setting
Inpatient rehabilitation unit at a large, academic medical center.
Participants
Adults with primary diagnosis of stroke, traumatic brain injury, or nontraumatic brain injury admitted to the inpatient rehabilitation unit between 2012 and 2017 (N=799).
Interventions
Not applicable.
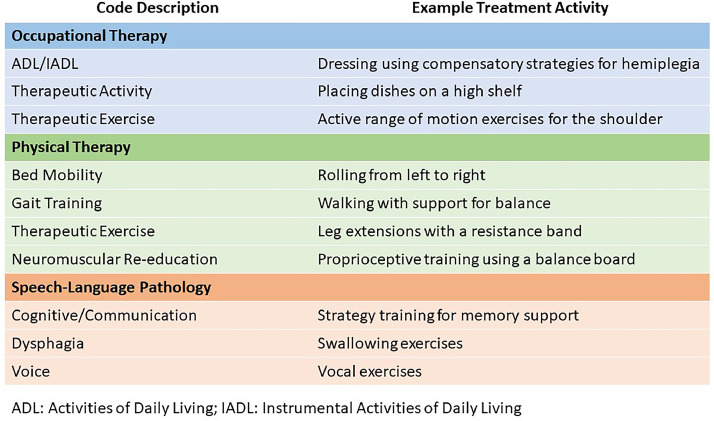
Main Outcome Measures
Gain rate in self-care and mobility function, using the Functional Independence Measure. Hierarchical regression models were used to identify the contributions of baseline characteristics, units, and content of occupational therapy, physical therapy, and speech-language pathology treatment to functional gain rates.
Results
Median length of rehabilitation stay was 10 days (interquartile range, 8-13d). Patients received an mean of 10.62 units of therapy (SD, 2.05) daily. For self-care care gain rate, the best-fitting model accounted for 32% of the variance. Occupational therapy activities of daily living units were positively associated with gain rate. For mobility gain rate, the best-fitting model accounted for 37% of the variance. Higher amounts of physical therapy bed mobility training were inversely associated with mobility gain rate.
Conclusions
More activities of daily living in occupational therapy is associated with faster improvement on self-care function for adults with acquired brain injury, whereas more bed mobility in physical therapy was associated with slower improvement. A potential challenge with value-based payments is the alignment between clinically appropriate therapy activities and the metrics by which patient improvement are evaluated. There is a risk that therapists and facilities will prioritize activities that drive improvement on metrics and deemphasize other patient-centered goals.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Archives of rehabilitation research and clinical translation
Medicine and Dentistry (General)
CiteScore
3.00
自引率
0.00%
发文量
0
审稿时长
8 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


