医疗保健相关感染的经济负担:意大利医疗保健设置的倾向评分分析。
IF 1.9
Q3 INFECTIOUS DISEASES
引用次数: 0
摘要
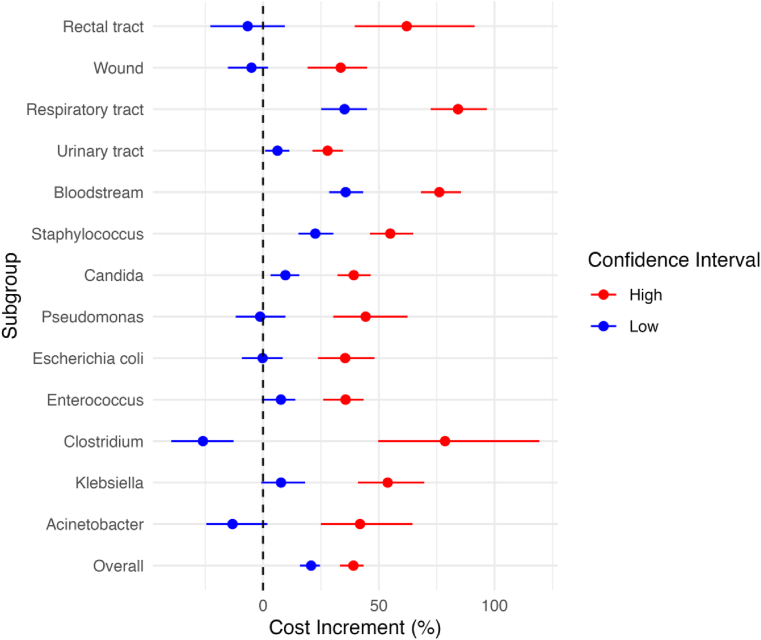
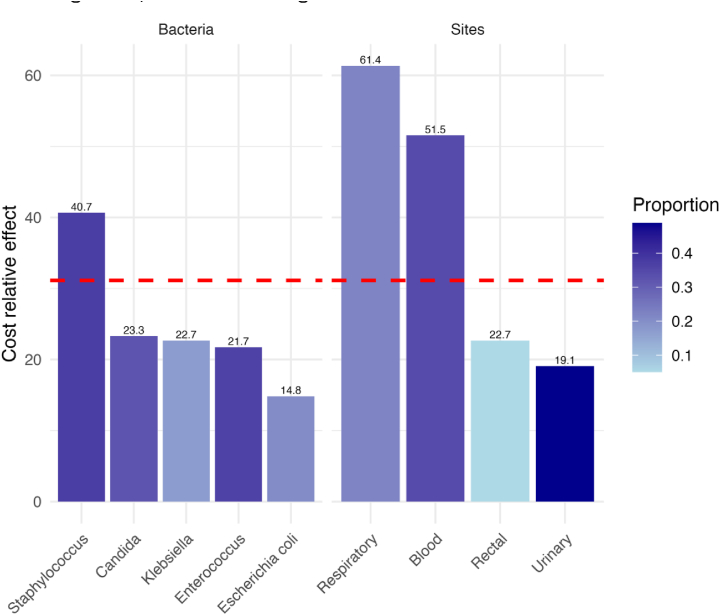
医院获得性感染(HAIs)是一个全球性的公共卫生挑战,影响患者安全,并在整个医疗保健环境中产生巨大的经济成本。本研究旨在通过分析与各种感染相关的实际成本,准确衡量HAIs的经济负担,为有针对性的预防和管理策略提供见解。方法:在意大利罗马的一所大学医院进行回顾性队列研究,分析2018年1月至12月的出院记录(HDR),重点是患有和不患有HAIs的患者。研究采用ICD-9-CM编码、微生物数据库、感染部位和微生物分层分析。使用DRG报销数据计算成本增量。倾向评分匹配比较了感染患者与匹配的非感染患者,通过两个模型模拟随机试验:一个模型调整住院时间和死亡率(不太保守),另一个模型不使用这些因素作为混杂因素(更保守)。结果:在polilinico Universitario Tor Vergata的12033名患者的研究中,10.07%的患者发展为HAI,显着提高了平均DRG 53.4%(€3,744至€5,744)。倾向得分分析显示,在一个模型中,HAIs使成本增加了4,695欧元(60.45%),在另一个模型中增加了3,335欧元(31.15%)。特定的微生物和感染地点进一步影响了成本影响,突出了有针对性的HAI预防战略的必要性。结论:我们的研究揭示了医院获得性感染(HAIs)的重大经济影响,与特定微生物和感染部位相关的成本大幅增加。这些发现强调需要有效的HAI预防策略,以提高患者安全并减少医疗保健支出。本文章由计算机程序翻译,如有差异,请以英文原文为准。
The financial burden of healthcare-associated infections: a propensity score analysis in an Italian healthcare setting
Introduction
Hospital-acquired infections (HAIs) present a global public health challenge, impacting patient safety and incurring substantial economic costs across healthcare settings. This study aims to accurately measure the financial burden of HAIs by analyzing real costs associated with various infections, providing insights for targeted prevention and management strategies.
Methods
This retrospective cohort study at a university hospital in Rome, Italy, analysed Hospital Discharge Records (HDR) from January to December 2018, focusing on patients with and without HAIs. The study employed ICD-9-CM codes, microbiology databases, and stratified analyses by infection site and microorganism. Cost increments were calculated using DRG reimbursement data. Propensity score matching compared infected patients with matched non-infected counterparts, simulating a randomized trial through two models: one adjusting for length of stay and mortality (less conservative), and one not using these factors as confounders (more conservative).
Results
In the study of 12,033 patients at Policlinico Universitario Tor Vergata, 10.07% developed an HAI, significantly raising mean DRG by 53.4% (€3,744 to €5,744). Propensity score analysis showed HAIs elevated costs by €4,695 (60.45%) in one model, and by €3,335 (31.15%) in another. Specific microbes and infection sites further influenced the cost impact, highlighting the need for targeted HAI prevention strategies.
Conclusion
Our study reveals the significant economic impact of hospital-acquired infections (HAIs), with a substantial increase in costs linked to specific microorganisms and infection sites. These findings highlight the need for effective HAI prevention strategies to enhance patient safety and reduce healthcare expenditures.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Infection Prevention in Practice
Medicine-Public Health, Environmental and Occupational Health
CiteScore
4.80
自引率
0.00%
发文量
58
审稿时长
61 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


