基于ct成像生物标志物的AI模型预测慢性乙型肝炎患者肝细胞癌
IF 26.8
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
背景,目的利用临床变量对慢性乙型肝炎(CHB)患者提出了多种肝细胞癌(HCC)预测模型。我们旨在通过结合来自腹部计算机断层扫描(CT)图像的成像生物标志物以及临床变量,开发基于人工智能(AI)的HCC预测模型。方法利用基于深度学习的CT自动分割软件DeepFore提取的成像生物标志物,建立基于梯度增强机器算法的人工智能预测模型。衍生队列(n=5,585)按3:1的比例随机分为训练集和内部验证集。外部验证队列包括2,883例患者。6项成像生物指标(腹部内脏脂肪-总脂肪体积比、总脂肪-躯干体积比、脾脏体积、肝脏体积);肝脾Hounsfield单位[HU]比值;选择8个临床变量作为我们的模型PLAN-B-DF的主要变量。结果在内部验证集中(中位随访时间为7.4年),PLAN-B-DF具有良好的预测性能,c指数为0.91,校正函数良好(Hosmer-Lemeshow检验P=0.78)。在外部验证队列(中位随访时间=4.6年)中,与PLAN-B、PAGE-B、改良PAGE-B和CU-HCC模型相比,PLAN-B- df具有更好的识别功能(c-index, 0.89 vs. 0.65-0.78;所有P<;0.001),并保持良好的校准函数(Hosmer-Lemeshow检验P=0.42)。根据PLAN-B-DF计算的风险概率将患者分为四组,最低、低、中、高风险组10年累积HCC发生率分别为0.0%、0.4%、16.0%和46.2%。结论该人工智能预测模型集成了基于深度学习的CT图像自动分割,在预测CHB患者HCC风险方面比以往的模型有更好的表现。影响和意义人工智能驱动的HCC预测模型(PLAN-B-DF)采用自动CT分割算法,在CHB患者的预测准确性和风险分层方面有显著提高。PLAN-B-DF使用梯度增强算法和CT指标,如内脏脂肪体积和肌骨化症,优于先前仅基于临床和人口统计数据的模型。与以往模型相比,该模型不仅显示出更高的c指数,而且有效地将CHB患者划分为不同的危险组。该模型利用机器学习分析导致HCC发生的各种危险因素之间的复杂关系,从而为CHB患者提供更加个性化的监测。本文章由计算机程序翻译,如有差异,请以英文原文为准。

AI model using CT-based imaging biomarkers to predict hepatocellular carcinoma in patients with chronic hepatitis B
Background & Aims
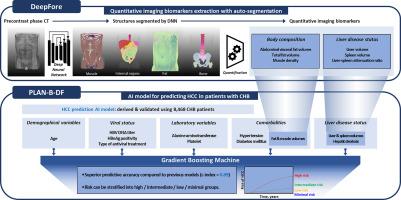
Various hepatocellular carcinoma (HCC) prediction models have been proposed for patients with chronic hepatitis B (CHB) using clinical variables. We aimed to develop an artificial intelligence (AI)-based HCC prediction model by incorporating imaging biomarkers derived from abdominal computed tomography (CT) images along with clinical variables.
Methods
An AI prediction model employing a gradient-boosting machine algorithm was developed utilizing imaging biomarkers extracted by DeepFore, a deep learning-based CT auto-segmentation software. The derivation cohort (n = 5,585) was randomly divided into the training and internal validation sets at a 3:1 ratio. The external validation cohort included 2,883 patients. Six imaging biomarkers (i.e. abdominal visceral fat–total fat volume ratio, total fat–trunk volume ratio, spleen volume, liver volume, liver–spleen Hounsfield unit ratio, and muscle Hounsfield unit) and eight clinical variables were selected as the main variables of our model, PLAN-B-DF.
Results
In the internal validation set (median follow-up duration = 7.4 years), PLAN-B-DF demonstrated an excellent predictive performance with a c-index of 0.91 and good calibration function (p = 0.78 by the Hosmer-Lemeshow test). In the external validation cohort (median follow-up duration = 4.6 years), PLAN-B-DF showed a significantly better discrimination function compared to previous models, including PLAN-B, PAGE-B, modified PAGE-B, and CU-HCC (c-index, 0.89 vs. 0.65–0.78; all p <0.001), and maintained a good calibration function (p = 0.42 by the Hosmer-Lemeshow test). When patients were classified into four groups according to the risk probability calculated by PLAN-B-DF, the 10-year cumulative HCC incidence was 0.0%, 0.4%, 16.0%, and 46.2% in the minimal-, low-, intermediate-, and high-risk groups, respectively.
Conclusion
This AI prediction model, integrating deep learning-based auto-segmentation of CT images, offers improved performance in predicting HCC risk among patients with CHB compared to previous models.
Impact and implications
The novel predictive model PLAN-B-DF, employing an automated computed tomography segmentation algorithm, significantly improves predictive accuracy and risk stratification for hepatocellular carcinoma in patients with chronic hepatitis B (CHB). Using a gradient-boosting algorithm and computed tomography metrics, such as visceral fat volume and myosteatosis, PLAN-B-DF outperforms previous models based solely on clinical and demographic data. This model not only shows a higher c-index compared to previous models, but also effectively classifies patients with CHB into different risk groups. This model uses machine learning to analyze the complex relationships among various risk factors contributing to hepatocellular carcinoma occurrence, thereby enabling more personalized surveillance for patients with CHB.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Hepatology
医学-胃肠肝病学
CiteScore
46.10
自引率
4.30%
发文量
2325
审稿时长
30 days
期刊介绍:
The Journal of Hepatology is the official publication of the European Association for the Study of the Liver (EASL). It is dedicated to presenting clinical and basic research in the field of hepatology through original papers, reviews, case reports, and letters to the Editor. The Journal is published in English and may consider supplements that pass an editorial review.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


