美学区即刻植入和即刻负荷后软硬组织的改变-系统回顾和荟萃分析。
IF 2.3
Q3 Dentistry
引用次数: 0
摘要
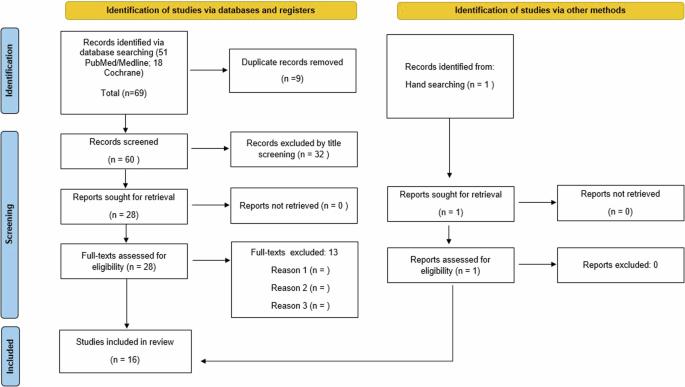
背景:I型即刻种植体具有治疗时间短、手术次数少、拔牙后骨质流失等优点,但由于角膜角化程度不够,对皮瓣适应构成挑战,阻碍了初级稳定性的实现。此外,科学证据支持拔牙后骨质流失是一种自然的生物现象,会影响治疗的成功。目的:主要目的是了解种植体即刻放置和即刻加载后周围硬软组织的变化。次要结果是记录种植体植入后的不良事件,如愈合过程中的感染和修复后的感染,种植体失败(包括手术和修复后)以及种植体的总体成功率和存活率。材料和方法:对2023年10月在线搜索引擎Medline/PubMed和Cochrane数据库中发表的英文文章进行详细的电子文献检索,不限制检索年份,包括立即种植体放置和加载的研究,平均随访时间至少为1年。采用反方差法对软硬组织变化进行加权均值分析。结果:共纳入16项研究。在上颌前牙即刻放置或延迟种植体即刻放置时,嵴骨水平无差异。与延迟种植体放置的病例相比,种植体周围边缘保持不变,乳头丢失无差异。无瓣入路比全厚瓣入路乳头更稳定或退缩更少。在骨移植材料填充GAP的研究中,骨水平变化未见明显变化。在退缩的情况下,即刻种植体放置与预备性确实导致大约1毫米少的面部牙龈退缩与组相比,有一个窝移植。即刻种植体置入术组比延迟种植体置入术组出现更多的种植体相关并发症。与延迟植入组相比,移植成功率和存活率几乎相似。结论:尽管与延迟种植体放置组相比,观察到相似的种植体存活率,但需要更多的长期研究来确定立即种植体放置和立即加载的成功。必须特别注意美学效果。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Soft and hard tissue changes following immediate implant placement and immediate loading in aesthetic zone—a systematic review and meta-analysis
Type I immediate implant placement has its own advantages like reduced treatment time, number of surgeries and post-extraction bone loss, however, the presence of insufficiently keratinized mucosa poses a challenge for flap adaptation and hinders the achievement of primary stability. Additionally, scientific evidence supports the notion that post-extraction bone loss is a natural biological occurrence that can impact the success of treatments. The primary outcome was to find out the hard and soft tissues changes around the implant following immediate placement and immediate loading. The secondary outcome was to record the adverse events post implant placement such as infection during the course of healing and after restoration, implant failure which would include surgical and post restoration, and over- all success and survival rate of implant. A detailed electronic literature search of the articles published in English language was undertaken in October 2023 on online search engines Medline/PubMed and Cochrane databases with no restriction on year of search to include studies on immediate implant placement and loading with a mean follow-up time of at least 1 year. Weighted means of soft and hard tissue changes were obtained by the inverse variance method. A total of 16 studies were included. There was no difference in crestal bone levels in immediate or delayed implant placement with immediate provisionalization in the anterior maxilla. The peri-implant margin remained and no differences in papillary loss was seen when compared to the delayed implant placement cases. Papilla were more stable or showed less recession in flapless approach compared to full thickness flap approach. Among the studies which filled the GAP with bone graft materials, no significant changes were found in the bone level changes. In case of recession, immediate implant placement with provisionalization did result in approximately 1 mm less facial gingival recession compared with that in the group that had a socket graft. Implant related complications occurred more in immediate implant placement and provisionalization compared to delayed group. And almost similar implant success and survival rates were seen in comparison to delayed implant placement groups. Despite the similar implant survival rates observed in comparison to delayed implant placement groups, more long-term studies are necessary to determine the success of immediate implant placement and immediate loading. Special attention has to be given to aesthetic outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Evidence-based dentistry
Dentistry-Dentistry (all)
CiteScore
2.50
自引率
0.00%
发文量
77
期刊介绍:
Evidence-Based Dentistry delivers the best available evidence on the latest developments in oral health. We evaluate the evidence and provide guidance concerning the value of the author''s conclusions. We keep dentistry up to date with new approaches, exploring a wide range of the latest developments through an accessible expert commentary. Original papers and relevant publications are condensed into digestible summaries, drawing attention to the current methods and findings. We are a central resource for the most cutting edge and relevant issues concerning the evidence-based approach in dentistry today. Evidence-Based Dentistry is published by Springer Nature on behalf of the British Dental Association.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


