具有全国代表性的美国成年人样本中心血管疾病和心血管健康与残疾状况的关系
IF 4.3
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
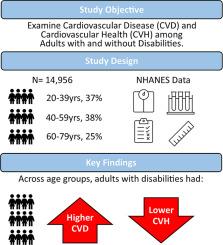
背景:需要更好地了解残疾成年人的心血管疾病(CVD)和心血管健康(CVH),以解决与残疾相关的健康差异问题。研究方法本研究分析了美国国家健康与营养检查调查(NHANES)的问卷、体检和 2013-2018 年的 24 小时饮食回忆数据,调查对象为年龄在 20-79 岁之间的自述残疾和非自述残疾成年人。心血管疾病根据自我报告进行二分法,而心血管健康则使用美国心脏协会生活必备 8 项(LE8)进行评估,包括四种健康行为(饮食、体育锻炼、尼古丁接触和睡眠健康)和四种健康因素(体重指数、血脂、血糖和血压),得分越高表示心血管健康越好。分析采用了复杂的多阶段 NHANES 抽样设计。研究结果该研究包括 1,300 名自我报告患有心血管疾病的成年人和 13,656 名无心血管疾病的成年人。对 20-39 岁、40-59 岁和 60-79 岁年龄组分别进行的加权逻辑回归表明,与无残疾的成年人相比,有残疾的成年人患心血管疾病的几率更高(ORadj (95 %CI) 分别为 8.0(4.6-14.1)、5.8(4.3-8.0)、2.5(1.9-3.3))。在无心血管疾病的人群中,就 LE8 总分(平均值为 56.9(0.5) vs. 65.7(0.3),p < .001)和所有八项 LE8 指标(p ≤ 0.004)而言,残疾人群的 CVH 低于非残疾人群。结论这些结果与改善残疾人健康和福祉的行动呼吁相一致,其中应包括针对饮食、体育活动、睡眠健康和戒烟等健康行为的福祉计划。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Association of cardiovascular disease and cardiovascular health with disability status in a nationally representative sample of US adults
Background: A better understanding of cardiovascular disease (CVD), and cardiovascular health (CVH) among adults with disabilities is needed to address disability related health disparities. Methods: This study analyzed National Health and Nutrition Examination Survey (NHANES) questionnaires, medical examinations, and 24-hour dietary recall data from 2013–2018 for adults age 20–79 years with and without self-reported disability. CVD was dichotomous based on self-report and CVH was assessed using American Heart Association Life's Essential 8 (LE8) comprised of four health behaviors (diet, physical activity, nicotine exposure, and sleep health) and four health factors (body mass index, blood lipids, blood glucose, and blood pressure) with higher scores indicating better CVH. Analyses incorporated the complex multistage NHANES sampling design. Results: The study included 1,300 adults with self-reported CVD and 13,656 adults who were CVD free. Separate weighted logistic regressions for age groups of 20–39, 40–59, and 60–79 years indicated adults with a disability had higher odds of CVD compared to those who were disability free (ORadj (95 %CI) 8.0(4.6–14.1), 5.8(4.3–8.0), 2.5(1.9–3.3) respectively). Among those who were CVD free, CVH was lower for those with a disability compared to those without a disability for the total LE8 score (meanadj(SE) 56.9(0.5) vs. 65.7(0.3), p < .001) and all eight LE8 metrics (p ≤ 0.004). Conclusion: These results are aligned with the call to action to improve health and wellness of persons with disabilities which should include wellness programming for health behaviors such as diet, physical activity, sleep health, and nicotine cessation.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American journal of preventive cardiology
Cardiology and Cardiovascular Medicine
CiteScore
6.60
自引率
0.00%
发文量
0
审稿时长
76 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


