儿童期总 IgE 水平与特异性 IgE 水平对比,用于定义和预测 T2 高哮喘
IF 3.9
2区 医学
Q2 ALLERGY
引用次数: 0
摘要
背景T2-高哮喘的特征是血嗜酸性粒细胞(b-eos)升高,和/或呼出一氧化氮(FeNO)分数升高,和/或 "过敏驱动",而 "过敏驱动 "尚未明确定义。方法 我们利用 COPSAC2000(n = 411)和 COPSAC2010(n = 700)母婴队列中的数据,重复测量了儿童时期的 tIgE、sIgE、b-eos 和 FeNO。我们通过 b-eos 升高(≥0.3 × 109/L)和/或 FeNO 升高(≥20 ppb)来定义 T2 高哮喘,并使用逻辑回归分析了 7/10/13/18 岁时 tIgE(特定年龄临界值)和 sIgE(≥0.35 kU/L)升高的相关性。此外,我们还使用逻辑回归和 ROC 模型分析了 0-4 岁时 tIgE 和 sIgE 升高与日后 T2 高哮喘风险之间的关联。使用Vuong似然比检验、Akaike或贝叶斯信息标准,总体上并不倾向于将tIgE和sIgE结合起来,而不是单独使用tIgE或sIgE。此外,0-4 岁时的 tIgE 升高与所有时间点的 T2 高哮喘风险相关(AUC = 0.63-0.70,灵敏度 = 0.62-0.81,特异性 = 0.57-0.78),而 0-4 岁时的 sIgE 升高仅与 18 岁时的 T2 高哮喘相关(AUC = 0.66,灵敏度 = 0.45,特异性 = 0.88)。tIgE和sIgE的AUC值无明显差异(DeLong检验)。本文章由计算机程序翻译,如有差异,请以英文原文为准。
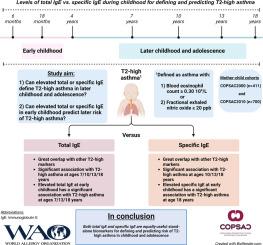
Levels of total IgE versus specific IgE during childhood for defining and predicting T2-high asthma
Background
T2-high asthma is characterized by elevated blood eosinophils (b-eos), and/or fractional exhaled nitric oxide (FeNO), and/or being “allergy-driven”, which is not well-defined.
Objective
To investigate the role of total and specific immunoglobulin E (tIgE/sIgE) for defining and predicting T2-high asthma in childhood as biomarkers of “allergy-driven”.
Methods
We utilized data from the COPSAC2000 (n = 411) and COPSAC2010 (n = 700) mother-child cohorts with repeated measurements of tIgE, sIgE, b-eos and FeNO through childhood. We defined T2-high asthma by elevated b-eos (≥0.3 × 109/L) and/or FeNO (≥20 ppb) and analyzed association with elevated tIgE (age-specific cut-offs) and sIgE (≥0.35 kU/L) using logistic regression at ages 7/10/13/18 years. Further, we analyzed the association between elevated tIgE and sIgE at age 0–4 years and later risk of T2-high asthma using logistic regression and ROC models.
Results
Elevated tIgE was associated with risk of T2-high asthma at all time points, whereas elevated sIgE showed similar results at ages 10/13/18 years. There was no overall model fit preference for a combination of tIgE and sIgE instead of tIgE or sIgE alone using Vuong's Likelihood-Ratio-Test, Akaike or Bayesian Information Criterion. Further, elevated tIgE at age 0–4 years was associated with later risk of T2-high asthma at all time points (AUC = 0.63–0.70, sensitivity = 0.62–0.81, specificity = 0.57–0.78), whereas elevated sIgE at 0–4 years was only associated with T2-high asthma at 18 years (AUC = 0.66, sensitivity = 0.45, specificity = 0.88). There were no significant differences in AUC values between tIgE and sIgE (DeLong's test).
Conclusion
Elevated tIgE and sIgE are equally useful stand-alone biomarkers for defining and predicting risk of T2-high asthma in childhood.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
World Allergy Organization Journal
Immunology and Microbiology-Immunology
CiteScore
9.10
自引率
5.90%
发文量
91
审稿时长
9 weeks
期刊介绍:
The official pubication of the World Allergy Organization, the World Allergy Organization Journal (WAOjournal) publishes original mechanistic, translational, and clinical research on the topics of allergy, asthma, anaphylaxis, and clincial immunology, as well as reviews, guidelines, and position papers that contribute to the improvement of patient care. WAOjournal publishes research on the growth of allergy prevalence within the scope of single countries, country comparisons, and practical global issues and regulations, or threats to the allergy specialty. The Journal invites the submissions of all authors interested in publishing on current global problems in allergy, asthma, anaphylaxis, and immunology. Of particular interest are the immunological consequences of climate change and the subsequent systematic transformations in food habits and their consequences for the allergy/immunology discipline.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


