利用小鼠胫骨骨膜骨化模型快速评估羟基磷灰石/霰石的成骨能力
IF 18
1区 医学
Q1 ENGINEERING, BIOMEDICAL
引用次数: 0
摘要
生物材料被广泛用作骨科植入物和骨移植替代物。我们旨在利用小鼠胫骨骨膜骨化模型开发一种快速成骨评估方法,以评估生物材料在 2-4 周内的骨形成/重塑潜力。将一种新型羟基磷灰石/霰石(HAA)生物材料植入 C57BL/6 小鼠的胫骨和胫骨前肌之间的并胫处。与假手术动物相比,14 天后可观察到快速的膜内骨形成,骨厚度和胼胝体体积增加了 4 到 8 倍(p < 0.0001),随后是骨重塑,植入 28 天后形成了一层新的皮质骨。在 HAA 中添加临床上常用的双膦酸盐唑来膦酸钠,在 28 天内促进新骨形成的效果明显优于单独使用 HAA(p < 0.01)。通过将 HAA 植入大鼠直径为 3.5 毫米的股骨松质骨缺损和迷你猪直径为 5 毫米的股骨皮质骨缺损,进一步证实了 HAA 的成骨潜力。为了了解细胞/生物材料界面的生物降解和细胞活性,对未脱钙的标本进行了树脂包埋,并对切片进行了扫描电子显微镜(SEM)/电子反向散射衍射(EBSD)/能量色散 X 射线光谱(EDS)联合分析。我们的结论是,小鼠胫骨骨膜骨化是快速评估生物活性材料与成骨组织相互作用的一种新方法。这项研究还突出表明,将碳酸钙与羟基磷灰石结合可增强生物降解和成骨作用。本文章由计算机程序翻译,如有差异,请以英文原文为准。
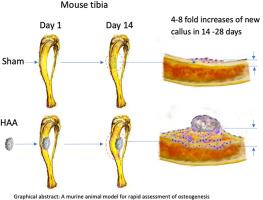
Rapid assessment of the osteogenic capacity of hydroxyapatite/aragonite using a murine tibial periosteal ossification model
Biomaterials are widely used as orthopaedic implants and bone graft substitutes. We aimed to develop a rapid osteogenic assessment method using a murine tibial periosteal ossification model to evaluate the bone formation/remodelling potential of a biomaterial within 2–4 weeks. A novel hydroxyapatite/aragonite (HAA) biomaterial was implanted into C57BL/6 mice juxtaskeletally between the tibia and tibialis anterior muscle. Rapid intramembranous bone formation was observed at 14 days, with 4- to 8-fold increases in bone thickness and callus volume in comparison with sham-operated animals (p < 0.0001), followed by bone remodelling and a new layer of cortical bone formation by 28 days after implantation. The addition of zoledronate, a clinically-utilised bisphosphonate, to HAA, promoted significantly more new bone formation than HAA alone over 28 days (p < 0.01). The osteogenic potential of HAA was further confirmed by implanting into a 3.5 mm diameter femoral cancellous bone defect in rats and a 5 mm diameter femoral cortical bone defect in minipigs. To understand the biodegradation and the cellular activity at the cell/biomaterial interfaces, non-decalcified specimens were resin embedded and sections subjected to combined scanning electron microscopy (SEM)/electron backscatter diffraction (EBSD)/energy dispersive X-ray spectrometry (EDS) analysis. We conclude that murine tibial periosteal ossification is a novel method for rapid assessment of the interaction of bioactive materials with osteogenic tissues. This study also highlights that combining calcium carbonate with hydroxyapatite enhances biodegradation and osteogenesis.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Bioactive Materials
Biochemistry, Genetics and Molecular Biology-Biotechnology
CiteScore
28.00
自引率
6.30%
发文量
436
审稿时长
20 days
期刊介绍:
Bioactive Materials is a peer-reviewed research publication that focuses on advancements in bioactive materials. The journal accepts research papers, reviews, and rapid communications in the field of next-generation biomaterials that interact with cells, tissues, and organs in various living organisms.
The primary goal of Bioactive Materials is to promote the science and engineering of biomaterials that exhibit adaptiveness to the biological environment. These materials are specifically designed to stimulate or direct appropriate cell and tissue responses or regulate interactions with microorganisms.
The journal covers a wide range of bioactive materials, including those that are engineered or designed in terms of their physical form (e.g. particulate, fiber), topology (e.g. porosity, surface roughness), or dimensions (ranging from macro to nano-scales). Contributions are sought from the following categories of bioactive materials:
Bioactive metals and alloys
Bioactive inorganics: ceramics, glasses, and carbon-based materials
Bioactive polymers and gels
Bioactive materials derived from natural sources
Bioactive composites
These materials find applications in human and veterinary medicine, such as implants, tissue engineering scaffolds, cell/drug/gene carriers, as well as imaging and sensing devices.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


