嗜睡症和特发性嗜睡症患者的社会支持和孤独感:一项国际调查。
IF 3.8
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
目的评估被诊断出患有嗜睡症或特发性嗜睡症时,在适应生活过程中感受到支持的相关因素:非营利组织 "睡眠项目 "通过电子邮件和社交网络发布了一项在线调查。调查对象为被诊断患有嗜睡症或特发性嗜睡症的成年人(≥18 岁)。采用多变量回归法来评估在适应这些病症的生活时是否感觉到支持的预测因素:共有 1308 人完成了调查(1 型嗜睡症患者占 48.4%;2 型嗜睡症患者占 28.7%;特发性嗜睡症患者占 22.9%)。总体而言,68.7%的受访者年龄在 40 岁以下;87.7%为女性;88.8%为白人。受访者居住在 38 个不同的国家(65.5% 在美国)。在确诊时,大多数受访者(91.1%)不认识患有相同疾病的人。在调查时,有 486 名受访者(37.2%)仍不认识任何患有相同诊断的人。只有 32.3% 的受访者在适应嗜睡症或特发性嗜睡症的生活时感到得到了支持。在接受调查时认识患有相同诊断的人是获得支持的一个重要预测因素。年龄较小(18-30 岁)和已婚也与感知到的支持度较高有关,而被诊断为 2 型嗜睡症或特发性嗜睡症(相对于 1 型嗜睡症)和居住在美国境外则与感知到的支持度较低有关:结论:嗜睡症或特发性嗜睡症患者通常不认识其他患有相同病症的人,尽管这与感受到的支持有关。临床医生应评估社会支持并协助识别资源。本文章由计算机程序翻译,如有差异,请以英文原文为准。
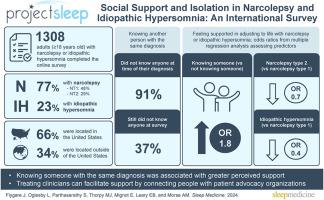
Social support and isolation in narcolepsy and idiopathic hypersomnia: An international survey
Objective
To evaluate factors associated with feeling supported in adjusting to life when diagnosed with narcolepsy or idiopathic hypersomnia.
Methods
An online survey was disseminated by nonprofit organization Project Sleep via email and social networks. Intended recipients were adults (≥18 years old) diagnosed with narcolepsy or idiopathic hypersomnia. Multivariable regression was used to assess predictors of feeling supported in adjusting to life with these conditions.
Results
The survey was completed by 1308 individuals (narcolepsy type 1, 48.4 %; narcolepsy type 2, 28.7 %; idiopathic hypersomnia, 22.9 %). Overall, 68.7 % of respondents were ≤40 years of age; 87.7 % were female; and 88.8 % were White. Respondents lived in 38 different countries (65.5 % in the United States). At time of diagnosis, most (91.1 %) did not know anyone with the same diagnosis. At time of the survey, 486 respondents (37.2 %) still did not know anyone with their diagnosis. Only 32.3 % of respondents felt supported in adjusting to life with narcolepsy or idiopathic hypersomnia. Knowing someone with the same diagnosis at the time of the survey was a significant predictor of perceived support. Younger age (18–30 years) and being married were also associated with greater perceived support, whereas a diagnosis of narcolepsy type 2 or idiopathic hypersomnia (versus narcolepsy type 1) and living outside the US were associated with less perceived support.
Conclusions
People with narcolepsy or idiopathic hypersomnia often do not know others living with the same condition, even though this is associated with feeling supported. Clinicians should assess for social support and assist with resource identification.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


