晚期肺气肿导致医疗点超声检查气胸假阳性率高。
IF 3.5
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
目的:护理点超声检查(POCUS)被广泛用于评估急性疾病的胸膜附着情况;然而,肺气肿患者中异常结果的发生率尚不清楚。本研究旨在描述晚期肺气肿患者 POCUS 结果的特征,并将实质和肺活量变化与异常 POCUS 结果相关联:我们对过度充气的 COPD 患者获得的 POCUS 图像进行了回顾性评估。图像在第 2 肋间(上叶)和膈肌插入上方(下叶)获得。胸膜滑动分为 "存在 "或 "不存在",M型图像分为 "海滨"、"条形码 "或 "混合 "模式;然后根据综合结果将患者分为四组。肺功能测试和高分辨率 CT 之间的差异通过 Chi Square 或方差分析进行检验,关联则通过 Spearman 相关性进行检验。三位评分者(两位肺科专家和一位放射科专家)之间的一致性采用 Kappa 统计法进行评估:我们的研究包括 48 名患者,共对 159 个肺叶进行了成像。我们发现相当一部分肺叶具有条形码 M 模式外观(13.8%)或肺滑动不确定/缺失(20.3%)。我们发现有 87 个肺叶(54.7%)不符合 M 型超声检查结果的任何典型定义。异常超声波模式与气流阻塞或肺气肿百分比无明显关联。三位分级人员的B型(0.20-0.611)和M型(0.24-0.049)之间存在较大的互异性:结论:过度充气患者在 POCUS 上经常出现胸膜滑动异常,条形码模式的假阳性率很高。在对 POCUS 进行解读以做出治疗决定时,应考虑到这一点。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Advanced emphysema leads to high false positivity rate for pneumothorax in point of care ultrasound
Purpose
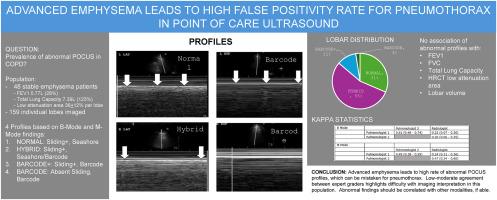
Point of Care Ultrasound (POCUS) is widely used to evaluate pleural apposition in acute disease; however, the prevalence of abnormal findings among emphysematous patients is unknown. The aim of the study was to characterize POCUS findings in advanced emphysema and correlate parenchymal and spirometric changes with abnormal POCUS results.
Materials and methods
We retrospectively evaluated POCUS images obtained in hyperinflated COPD patients. Images were obtained in the 2nd intercostal space (upper lobes) and above diaphragm insertion (lower lobes). Pleural sliding was graded as “present” or “absent,” and M-mode images graded as “seashore,” “barcode,” or “hybrid” patterns; patients were then assigned to four groups based on the combination of findings. Differences between pulmonary function testing and high-resolution CT were made by Chi Square or ANOVA testing, and association by Spearman's correlation. Agreement among three scorers (two pulmonologists and one radiologist) was assessed using Kappa statistics.
Results
Our study included 48 patients with 159 lobes imaged. We found a substantial percentage of lobes had either barcode M-mode appearance (13.8 %) or indeterminate/absent lung sliding (20.3 %). We identified 87 lobes (54.7 %) that did not fit any typical definition for M-mode ultrasound findings. There was no strong association of abnormal ultrasound patterns with airflow obstruction or emphysema percentage. There was wide interrater variability among B-mode (0.20–0.611) and M-mode (0.24-0.049) among the three graders.
Conclusions
Hyperinflated patients often show abnormal pleural sliding appearance on POCUS, with a high false positive rate of barcode pattern. This should be considered when interpretation of POCUS drives therapeutic decisions.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Respiratory medicine
医学-呼吸系统
CiteScore
7.50
自引率
0.00%
发文量
199
审稿时长
38 days
期刊介绍:
Respiratory Medicine is an internationally-renowned journal devoted to the rapid publication of clinically-relevant respiratory medicine research. It combines cutting-edge original research with state-of-the-art reviews dealing with all aspects of respiratory diseases and therapeutic interventions. Topics include adult and paediatric medicine, epidemiology, immunology and cell biology, physiology, occupational disorders, and the role of allergens and pollutants.
Respiratory Medicine is increasingly the journal of choice for publication of phased trial work, commenting on effectiveness, dosage and methods of action.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


