早期妊娠糖尿病后的产后血糖异常:TOBOGM随机对照试验中妇女的随访。
IF 6.1
3区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
目的:评估妊娠20周前患早期妊娠糖尿病(eGDM)的高危产妇产后血糖异常的发生率和预测因素:本研究是 "妊娠期糖尿病预约治疗(TOBOGM)研究 "的一项子研究。"妊娠期糖尿病预约治疗(TOBOGM)研究 "是一项随机对照试验,根据目前世界卫生组织的标准,对具有糖尿病危险因素并被诊断为 eGDM 的妇女进行早期或延迟治疗。妊娠合并糖尿病不包括在内。建议在产后 6-12 周再次进行口服葡萄糖耐量试验(oGTT):结果:在 793 名参与者中,352 人(44.4%)接受了产后口服葡萄糖耐量试验。进行和未进行 oGTT 的参与者的基线特征相似。92人(26.1%)患有产后血糖异常:11人(3.1%)患有糖尿病,31人(8.8%)患有空腹血糖受损(IFG),39人(11.1%)患有糖耐量受损(IGT),11人(3.1%)合并IFG/IGT。产后血糖异常的参与者更有可能既往患有 GDM、体重指数较低、妊娠体重增加较多、孕早期 oGTT 的 1 小时和 2 小时血糖浓度较高。在逻辑回归中,1 小时和 2 小时血糖浓度较高、曾患过 GDM 和妊娠体重增加较多与产后血糖异常有独立关联:结论:在患有 eGDM 的高危产妇中,产后血糖异常的发生率很高。本文章由计算机程序翻译,如有差异,请以英文原文为准。
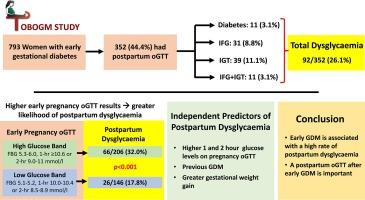
Postpartum dysglycaemia after early gestational diabetes: Follow-up of women in the TOBOGM randomised controlled trial
Aim
To evaluate the incidence and predictors of postpartum dysglycaemia among high-risk women who develop early gestational diabetes (eGDM) prior to 20 weeks’ gestation.
Methods
This is a sub-study of the Treatment of Booking Gestational Diabetes (TOBOGM) Study, a randomised controlled trial of early or deferred treatment for women with risk factors for gestational diabetes diagnosed with eGDM, using current WHO criteria. Overt diabetes in pregnancy was excluded. A repeat oral glucose tolerance test (oGTT) was recommended at 6–12 weeks postpartum.
Results
Of 793 participants, 352 (44.4%) underwent a postpartum oGTT. Baseline characteristics of participants with and without an oGTT were similar. Ninety-two (26.1%) had postpartum dysglycaemia: 11 (3.1%) diabetes, 31 (8.8%) impaired fasting glucose (IFG), 39 (11.1%) impaired glucose tolerance (IGT), and 11 (3.1%) combined IFG/IGT. Participants with postpartum dysglycaemia were more likely to have had past GDM, lower body mass index, more gestational weight gain, and higher 1 and 2-hour glucose concentrations on the early pregnancy oGTT. On logistic regression, higher 1 and 2-hour glucose concentration, previous GDM and greater gestational weight gain were independently associated with postpartum dysglycaemia.
Conclusion
There is a high incidence of postpartum dysglycaemia among high-risk women with eGDM.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Diabetes research and clinical practice
医学-内分泌学与代谢
CiteScore
10.30
自引率
3.90%
发文量
862
审稿时长
32 days
期刊介绍:
Diabetes Research and Clinical Practice is an international journal for health-care providers and clinically oriented researchers that publishes high-quality original research articles and expert reviews in diabetes and related areas. The role of the journal is to provide a venue for dissemination of knowledge and discussion of topics related to diabetes clinical research and patient care. Topics of focus include translational science, genetics, immunology, nutrition, psychosocial research, epidemiology, prevention, socio-economic research, complications, new treatments, technologies and therapy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


