对作为高危人群的吸烟者进行胰腺癌筛查:前瞻性队列研究的系统回顾和荟萃分析
引用次数: 0
摘要
目的:本研究的主要目的是对前瞻性队列研究的总体数据进行系统综述和荟萃分析,以确定吸烟影像筛查与胰腺癌(PC)早期诊断之间的关联:1) 在人类中进行的前瞻性队列研究;2) 适当的成像筛查方法;3) 参与者被归类为吸烟高危人群,且无 PC 遗传倾向的报告;4) 既往未确诊 PC;5) 在基线筛查后检测并诊断出腺癌的研究;6) 可获得主要结果 PC 的数据;7) 1992 年 1 月 1 日至 2024 年 7 月 22 日期间以英语发表的研究。不符合上述所有标准的研究均被排除在外。信息来源包括1) PubMed、2) CINAHL、3) Scopus、4) Cochrane 对照试验中央登记册 (CENTRAL)、5) NIH 国家癌症研究所癌症预防部、6) 胰腺癌行动网络、7) ProQuest、8) 英国医学杂志肠道与胰腺学、9) Clinicaltrials.gov。最后一次检索(PubMed)的日期为 2024 年 7 月 22 日。偏倚风险采用 Cochrane Collaborations Risk Of Bias In Non-randomized Studies of Exposures [2] 工具进行评估。小规模研究效应(发表偏倚等)采用 Doi 图和 LFK 指数进行评估。主要结果 PC 的效应大小指标为几率比(OR)。采用逆方差(IVhet)模型对奇数比进行汇总。采用建议、评估、发展和评价分级(GRADE)工具对证据的强度/确定性进行评估。五项研究中有两项报告了吸烟者的确切诊断阶段。在胰腺癌病例(n = 34)中,吸烟的估计效应表明吸烟有害(OR = 2.24,95 % CI,0.96 至 5.23),但统计学意义较弱(p = 0.06)。在统计学上观察到明显的异质性(Q = 11.1,P = 0.03)和中度不一致性(I2 = 63.9 %,95 % CI,5.0 至 86.3 %)。95 % 预测区间 (PI) 为 0.15 至 32.38。基于 ROBINS-E 的偏倚风险从高到非常高不等,基于 GRADE 评估的证据确定性非常低。结论虽然没有统计学意义,但我们的研究结果表明吸烟者患胰腺癌的几率可能会增加。然而,在解释这些发现时,需要考虑到所观察到的高偏倚风险和极低的证据确定性。在得出明确结论之前,还需要进行更多设计良好的研究,包括对吸烟和其他高危人群筛查方法的有意评估,以支持临床指南的制定。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Screening for pancreatic cancer among smokers as high-risk individuals: Systematic review and meta-analysis of prospective cohort studies
Objective
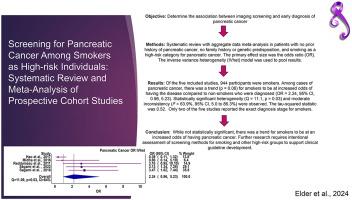
The main objective of this study was to conduct an aggregate data systematic review with meta-analysis of prospective cohort studies to determine the association between imaging screening for smoking and early diagnosis of pancreatic cancer (PC).
Methods
Eligible studies included the following: 1) prospective cohort studies conducted in humans, 2) appropriate imaging screening method, 3) participants categorized into smoking as a high-risk group with no reported genetic disposition for PC, 4) no prior diagnosis of PC, 5) studies which detected and diagnosed adenocarcinoma following baseline screening, 6) data available for our primary outcome, PC, 7) studies published in the English language from January 1, 1992 to July 22, 2024. Any studies not meeting all of the above criteria were excluded. Information sources included the following: 1) PubMed, 2) CINAHL, 3) Scopus, 4) Cochrane Central Register of Controlled Trials (CENTRAL), 5) NIH National Cancer Institute's Division of Cancer Prevention, 6) Pancreatic Cancer Action Network, 7) ProQuest, 8) The British Medical Journal's Gut and Pancreatology, 9) Clinicaltrials.gov. The date of the last search (PubMed) was conducted on July 22, 2024. Risk of bias was assessed using the Cochrane Collaborations Risk Of Bias In Non-randomized Studies of Exposures [2] instrument. Small-study effects (publication bias, etc.) was assessed using the Doi plot and LFK index. The effect size metric for the primary outcome, PC, was the odds ratio (OR). Odd's ratios were pooled using the inverse-variance (IVhet) model. The strength/certainty of evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) instrument.
Results
Five retrospective cohort studies representing 3,517 patients met the criteria for inclusion, 944 of whom were smokers. Two of the five studies reported the exact diagnosis stage for smokers. Among cases of pancreatic cancer (n = 34), the estimated effect of smoking suggested harm (OR = 2.24, 95 % CI, 0.96 to 5.23) though with weak statistical significance (p = 0.06). Statistically significant heterogeneity (Q = 11.1, p = 0.03) and moderate inconsistency (I2 = 63.9 %, 95 % CI, 5.0 to 86.3 %) were observed. The 95 % prediction interval (PI) was 0.15 to 32.38. Risk of bias, based on ROBINS-E ranged from high to very high, with very low certainty of evidence based on the GRADE assessment.
Conclusions
While not statistically significant, our findings suggest that smokers may be at an increased odds of having pancreatic cancer. However, these findings need to be interpreted with respect to the high risk of bias and very low certainty of evidence observed. A need exists for additional, well-designed studies that include intentional assessment of screening methods for smoking and other high-risk groups to support clinical guideline development before any definitive conclusions can be drawn.
Sources of funding
No funding was received for this work.
Registration
An a priori protocol was developed but not registered in any registry because of concerns about plagiarism.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Health sciences review (Oxford, England)
Medicine and Dentistry (General)
自引率
0.00%
发文量
0
审稿时长
75 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


